Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- 参考文献 Reference
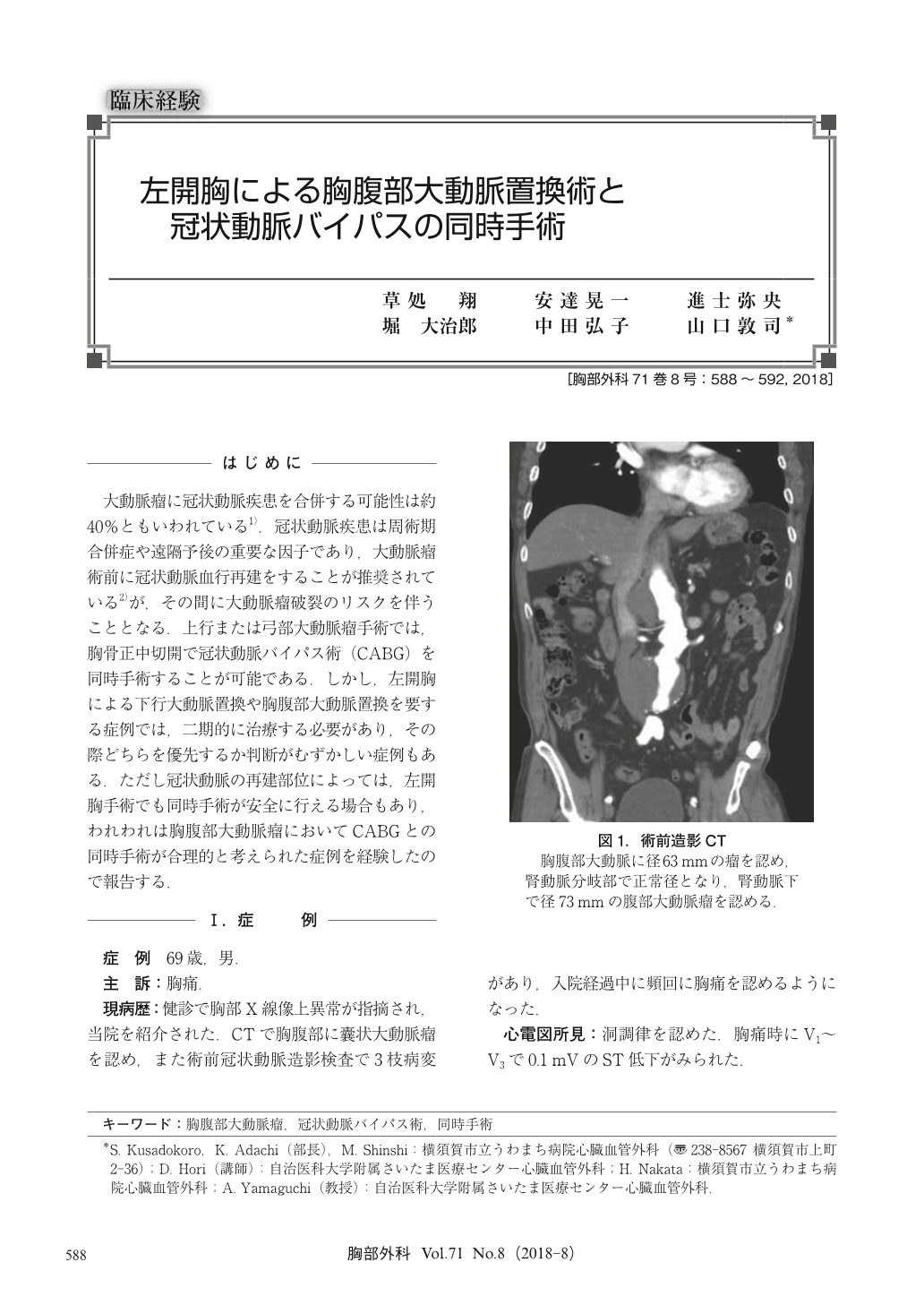
大動脈瘤に冠状動脈疾患を合併する可能性は約40%ともいわれている1).冠状動脈疾患は周術期合併症や遠隔予後の重要な因子であり,大動脈瘤術前に冠状動脈血行再建をすることが推奨されている2)が,その間に大動脈瘤破裂のリスクを伴うこととなる.上行または弓部大動脈瘤手術では,胸骨正中切開で冠状動脈バイパス術(CABG)を同時手術することが可能である.しかし,左開胸による下行大動脈置換や胸腹部大動脈置換を要する症例では,二期的に治療する必要があり,その際どちらを優先するか判断がむずかしい症例もある.ただし冠状動脈の再建部位によっては,左開胸手術でも同時手術が安全に行える場合もあり,われわれは胸腹部大動脈瘤においてCABGとの同時手術が合理的と考えられた症例を経験したので報告する.
Approximately 40% of the patients with aortic aneurysm have coronary artery disease(CAD), which is an important factor contributing to early mortality associated with aneurysm surgery. Combined coronary artery bypass grafting(CABG)and aortic aneurysm repair of the ascending aorta to the aortic arch is often performed through a median sternotomy due to a good surgical exposure. However, treatment strategy of thoraco-abdominal aortic aneurysm(TAAA)combined with CAD is often controversial. We report a successful case of a 69-year-old man who underwent TAAA repair and CABG through a left thoracotomy. Left thoracotomy via the 5th intercostal space with para-rectal incision provides a good surgical exposure of the thoraco-abdominal aorta and the left anterior descending artery(LAD). LAD was revascularized with a saphenous vein graft which was anastomosed to the descending aorta, followed by TAAA repair. The postoperative course was uneventful and the patient was discharged on 13th postoperative day without any complications.
© Nankodo Co., Ltd., 2018


