Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
実験水頭症犬(kaolin-induced hydrocephalus)のCTにおけるPVL (periventricular lucency)について,Metrizamide脳室造影およびcontrast enhancementの併用,V-P shunt手術前後の観察,病理学的検索を行い,その成因を検討した。
In clinical cases, pathogenesis of periventricular lucency (PVL) in computed tomography (CT) have been regarded as a periventricular edema by trans-ependymal egress of CSF during increased intra-ventricular pressure. But, in the study of CT in experimental canine hydrocephalus, PVL was observed also in the chronic stage, or on the contrary, PVL was sometimes impossible to be found in the acute hypertensive hydrocephalus. Even in clinical cases other than hydrocephalus, PVL was observed in other diseases which had no increased intraventricular pressure. The PVL in these cases can not be regarded just as a peri-ventricular edema.
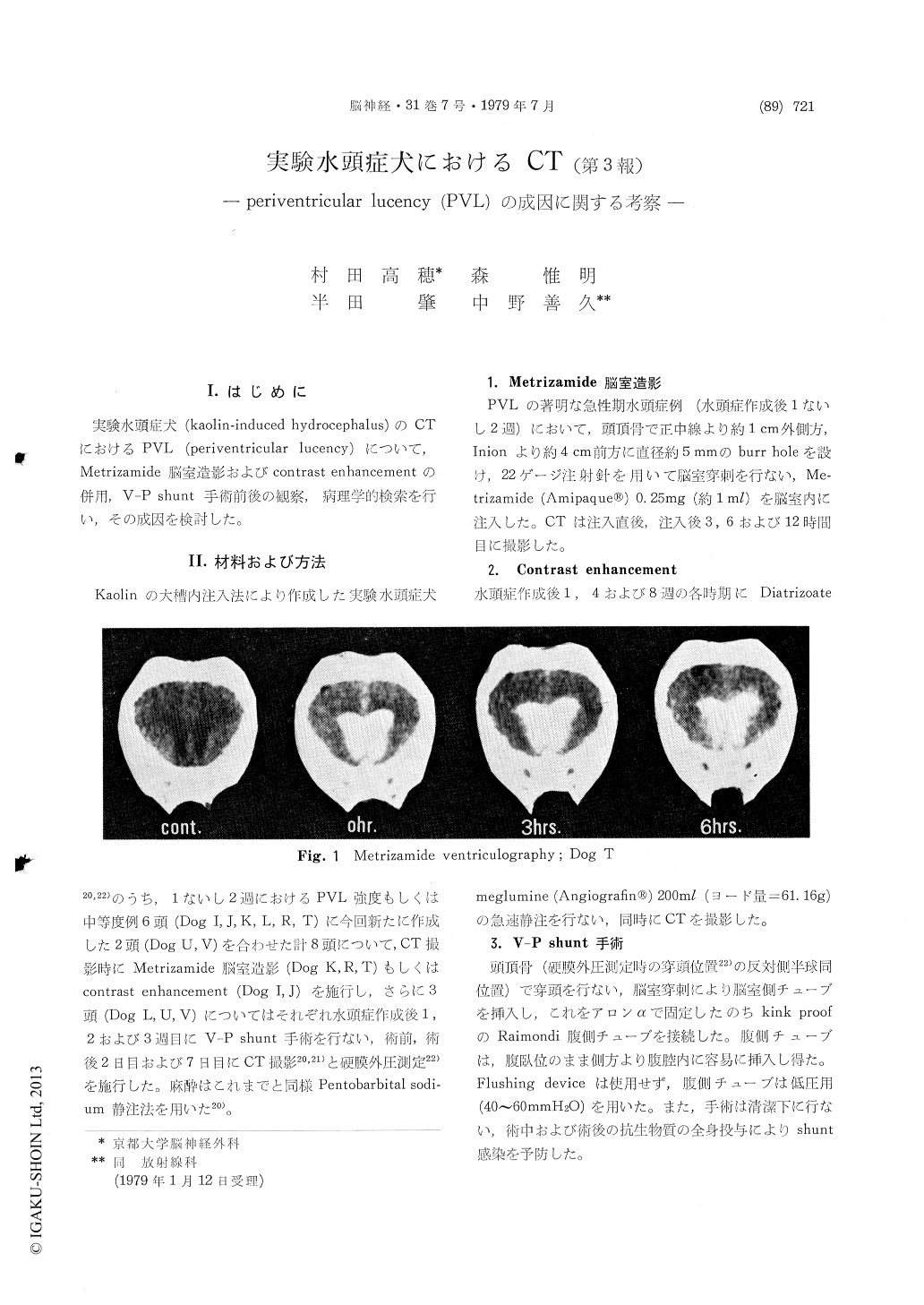
In this paper, we will discuss PVL in CT ex-perimental study. We investigated Metrizamide (AmipaqueR) ventriculography and contrast en-hancement. Furthermore, we performed V-P shunting operations and checked CT scans andepidural pressure (EDP) monitorings before and after operations. In addision, we studied light microscopic histological examinations at the superolateral angle of frontal horn in the lateral ventricles. There were spongy and edematous changes in the subependymal white matter, which we could identify with PVL on CT.
In Metrizamide ventriculography, contrast ma-terial in the ventricles passed through the ven-tricular ependym and gradually came into the periventricular white matters. The permeation of Metrizamide was considered to be a subsidary transependymal CSF egress in hydrocephalus. According to the study of printout data, an increase of the numerical value on CT numbers were more marked in PVL than that in other periventricular tissues. This finding suggests that transependymal CSF egress has been more remarkable in the PVL area than the other areas. These results are con-sistent with the following, that PVL is the most remarkable at the superolateral angle of frontal horn in the lateral ventricles on CT.
In contrast enhancement study, PVL was slightly enhanced. This might be due to poor circulation of blood on PVL because of high water content in the extracellular spaces and high tissue pressure by increased intraventricular pressure.
PVL was marked on CT in the acute hypertensive hydrocephalus, but immediately disappeared after V-P shunting operation (in 2 days), and PVL appeared again by shunt malfunction (in 1 week), when the ventricular system enlarged and EDP increased again. These sudden and reversible changes on CT were impossible to explain by production and destruction of protein or lipid, but were considered to be a change of water content.
From the forgoing, the pathogenesis of PVL on CT were examined. We ascertain that PVL on acute hypertensive hydrocephalus which is regarded as a pressure sign on CT, is a periventricular edema by transependymal CSF egress At the present time, the pathogenesis of PVL in the chronic stage or on non-hypertensive hydrocephalus are still unknown, but those are considered to be irreversible changes by periventricular infarctions that have been induced in the preceding hypertensive period.
In the future, we will investigate various PVL in clinical cases once again, and in experimental study, investigate the pathological changes of microvascular architecture around ventricles, par-ticularly in PVL.
Copyright © 1979, Igaku-Shoin Ltd. All rights reserved.


