Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
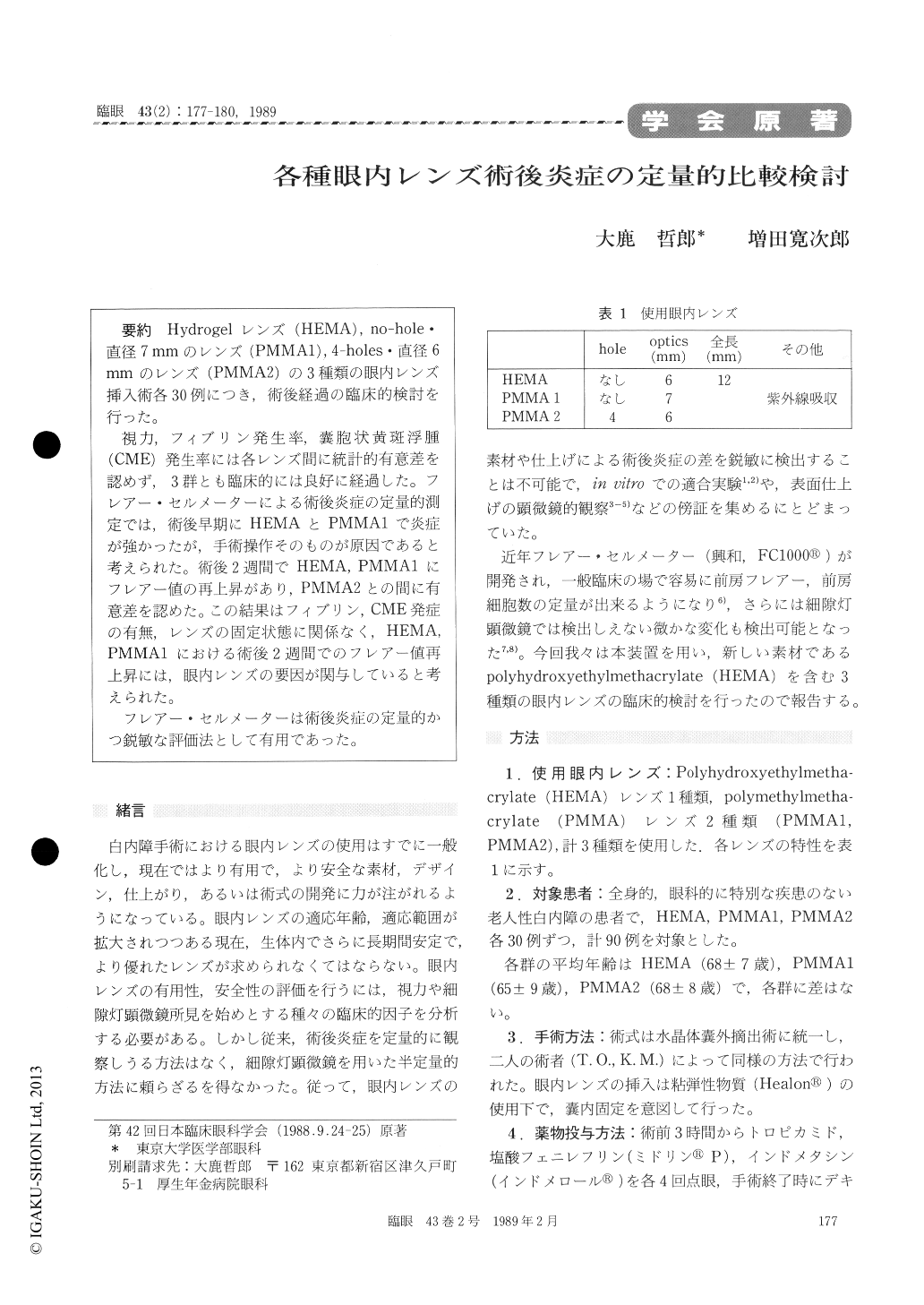
Hydrogelレンズ(HEMA),no-hole・直径7mmのレンズ(PMMAI),4—holes・直径6mmのレンズ(PMMA2)の3種類の眼内レンズ挿入術各30例につき,術後経過の臨床的検討を行った。
視力,フィブリン発生率,嚢胞状黄斑浮腫(CME)発生率には各レンズ間に統計的有意差を認めず,3群とも臨床的には良好に経過した。フレアー・セルメーターによる術後炎症の定量的測定では,術後早期にHEMAとPMMA1で炎症が強かったが,手術操作そのものが原因であると考えられた。術後2週間でHEMA, PMMA1にフレアー値の再上昇があり,PMMA2との間に有意差を認めた。この結果はフィブリン,CME発症の有無レンズの固定状態に関係なく,HEMA, PMMA1における術後2週間でのフレアー値再上昇には,眼内レンズの要因が関与していると考えられた。
フレアー・セルメーターは術後炎症の定量的かつ鋭敏な評価法として有用であった。
We evaluated three different types of intraocular lens (IOL) using postsurgical inflammation as parameter. Three groups consisting of 30 eyes each received different IOLs : HEMA IOL, PMMA1 IOL (no hole, 7 mm diameter, UV -cut), and PMMA2 IOL (4 holes, 6 mm diameter). The eyes were foll-owed up for 6 months postoperatively.
There was no difference among the 3 groups concerning visual acuity, fibrin deposit or incidence of cystoid macular edema. Overall clinical results were satisfactory in all the groups.
We quantitated the aqueous flare intensity and number of cells using a flare-cell mater. Flare value and number of cells in the early postoperative period were higher in HEMA and PMMA1 group than in the PMMA2 group. This difference could be attributed to the operative maneuvers. In the 2nd postoperative week, the flare values in HEMA and PMMA1 groups increased to form a peak signifi-cantly higher than in the PMMA2 group. There was a same tendency when the flare value was reanal-yzed excluding cases with fibrinous exudation, cystoid macular edema or without proper in-the -bag fixation. The difference in the type of IOL seemed to play a role in the above finding.
Copyright © 1989, Igaku-Shoin Ltd. All rights reserved.


