Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
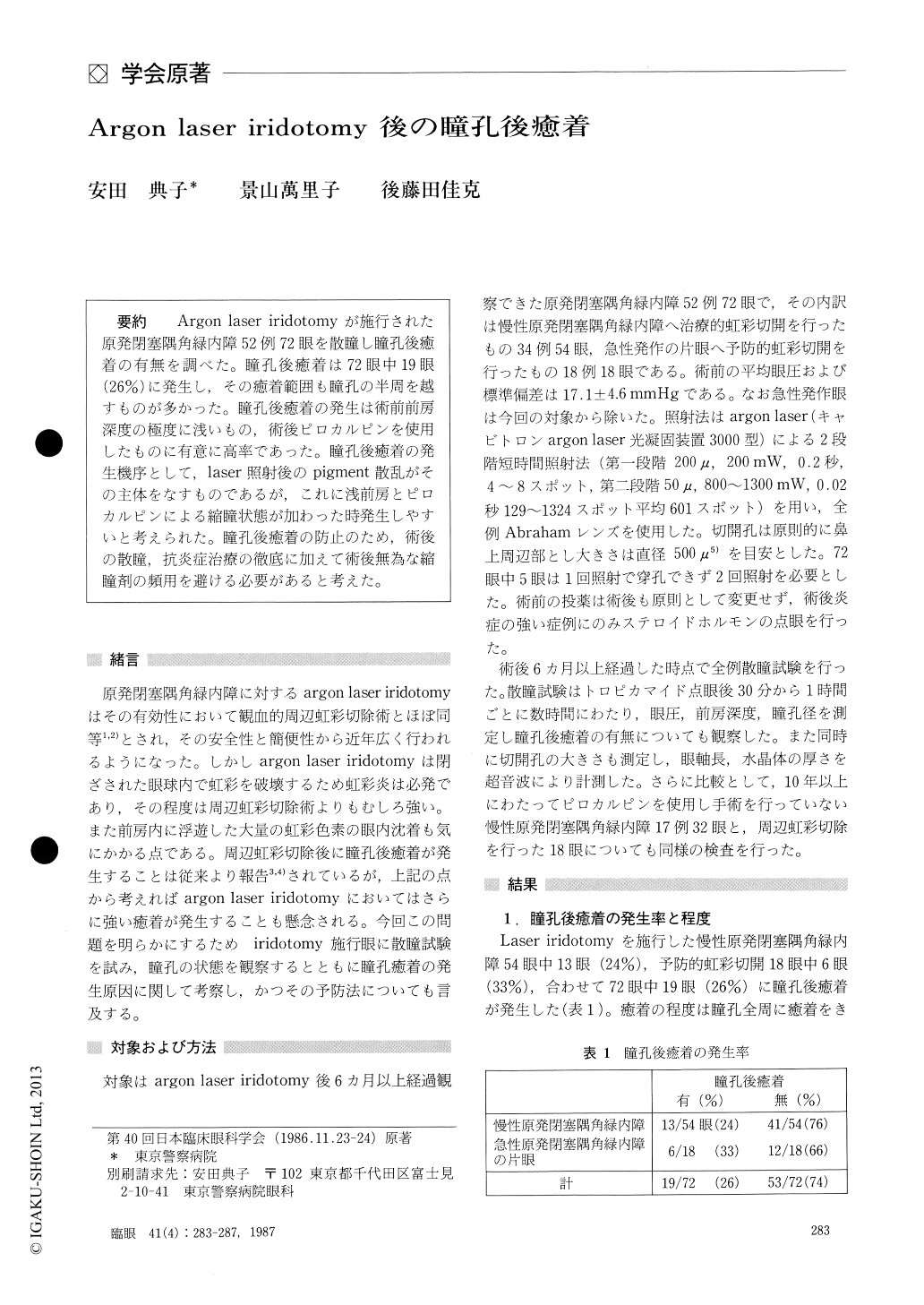
Argon laser iridotomyが施行された原発閉塞隅角緑内障52例72眼を散瞳し瞳孔後癒着の有無を調べた.瞳孔後癒着は72眼中19眼(26%)に発生し,その癒着範囲も瞳孔の半周を越すものが多かった.瞳孔後癒着の発生は術前前房深度の極度に浅いもの,術後ピロカルピンを使用したものに有意に高率であった.瞳孔後癒着の発生機序として,laser照射後のpigment散乱がその主体をなすものであるが,これに浅前房とピロカルピンによる縮瞳状態が加わった時発生しやすいと考えられた.瞳孔後癒着の防止のため,術後の散瞳,抗炎症治療の徹底に加えて術後無為な縮瞳剤の頻用を避ける必要があると考えた.
Mydriasis test was performed on 72 eyes in 52 patients treated by argon laser iridotomy for pri-mary chronic angle closure glaucoma.
Posterior synechia was present in 19 eyes (26%). The synechia involved more than 180° of the pupil-lary area. The incidence of synechia was greater in patients with shallow anterior chamber and in those with topical pilocarpine therapy follwing laser iridotomy.
Posterior synechia seemed to be the conseqence ofpigment dispersion during laser iridotomy proce-dure. Other factors, such as shallow anterior cham-ber and pilocarpine-induced miosis, would facilitate formation of synechia.
In order to prevent posterior synechia, mydriasis and topical steroid is advocated after laser iridotomy till signs of iritis disappear. Instillation of miotics should be discontinued after laser iridotomy.
Rinsho Ganka (Jpn J Chn Ophthalmol) 41(4) : 283-287, 1987
Copyright © 1987, Igaku-Shoin Ltd. All rights reserved.


