Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
慢性硬膜下血腫は,臨床上経験することの多い症患であり,CTスキャンによる診断,頭蓋穿孔よりの血腫内容の排除,洗滌など,診断,治療に関しては,おおよそ解決されているが,その発生機序については,1857年Virchowの炎症説に始まり,数多くの学説が出され2,5),多くは外傷に起因するという説にかたむいてはいるが,いまだに,その特異な発生過程--特に外傷性血腫でありながら,きわめて慢性の発生過程をとるという機序--は充分に解明されていない。
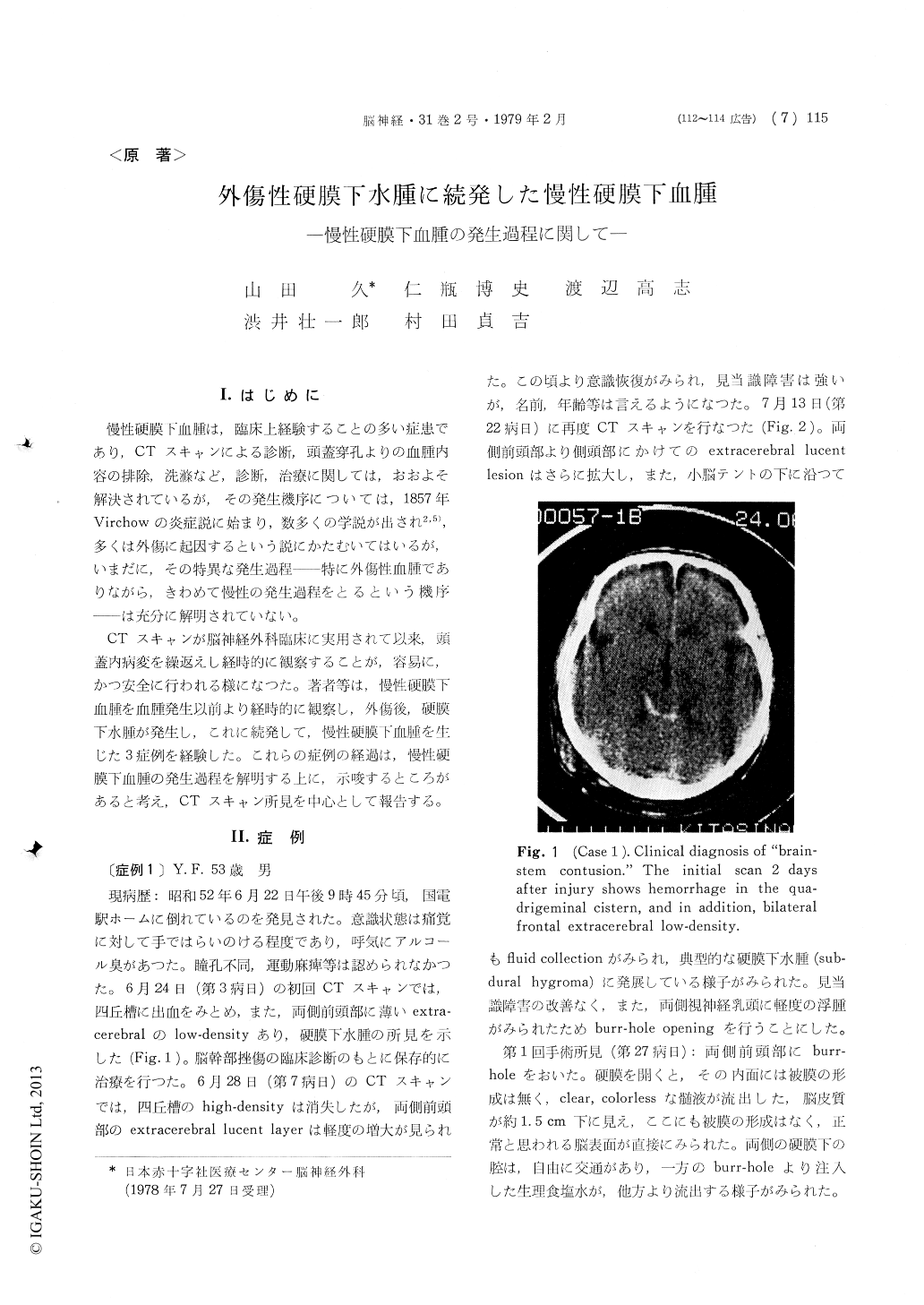
CTスキャンが脳神経外科臨床に実用されて以来,頭蓋内病変を繰返えし経時的に観察することが,容易に,かつ安全に行われる様になつた。著者等は,慢性硬膜下血腫を血腫発生以前より経時的に観察し,外傷後,硬膜下水腫が発生し,これに続発して,慢性硬膜下血腫を生じた3症例を経験した。これらの症例の経過は,慢性硬膜下血腫の発生過程を解明する上に,示唆するところがあると考え,CTスキャン所見を中心として報告する。
Follow-up CT-scan findings of three cases of chronic subdural hematoma occurring consequently to the posttraumatic subdural hygroma are presented. Case 1 was a 53 year old man who had sustained a moderately severe head injury suggesting brainstem contusion. Bilateral delayed subdural hygroma developed and was confirmed at operation 27 days after the injury. The hygroma did not have any capsule. Later, a chronic subdural hematoma developed on the left side two-months after injury within a period of 45 days. The hematoma was expanding and encapsulated. One hundred and eighty ml of hematoma content were obtained from a frontal burr-hole.
In the second case (76 year old male) who had a mild head injury, a similar bilateral hygroma was demonstrated 32 days after the injury. The CT-scan on the 54th day showed bilateral extra-cerebral narrow high-density lesion. In the following 16 days, an encapsulated subdural hematoma of iso-density had developed on the left side. High-density extracerebral lesion was still seen at the right fronto-temporal region. The patient had deteriolated on the 73rd day and was operated. The volume of the hematomas were estimated to be 100 ml on the left and 40 ml on the right side.
A subdural hematoma was formed in the 3rd cases, a 68 year old man, who had a moderate head injury. The initial CT-scan showed a thin extra-cerebral high-density layer localized at the right temporal area. Right frontal extracerebral low-density lesion, presumably an unilateral post-traumatic subdural hygroma, was revealed on the 10th day and, again, on the 18th day. Repeat-scan 49 days after the injury revealed a subdural hematoma at the site of the hygroma. The hematoma was formed within 23 days at maximum.
In all of these three cases the chronic subdural hematoma had developed consequently to the post-traumatic subdural hygroma in a relatively short period of 2 to 3 weeks. Whether this clinical sequence is peculiar to these three cases reported here, or common to the chronic subdural hematomas,is yet to determine in future studies, though, it seems to give an explanation to some of the baffling nature of the chronic subdural hematomas.
French et al. reported CT-scan findings of the posttraumatic subdural hygroma similar to these cases. The experimental condition and subacute development of the subdural hematomas produced in the experimental animical by Watanabe et al., seems to be materialized in our clinical cases. From their histopathological studies on the age of the hematoma membrane, Sakaki et al. believe that the development of the chronic subdural hematoma should start not at the time immediate after the head injury, but, rather, from the time of clinicalmanifestation of symptoms. These results are understandable if a proceeding subdural hygroma is postulated.
These three cases of chronic subdural hematoma suggest that the posttraumatic subdural hygroma have, at least, a close relation to the genesis of the chronic subdural hematoma. The authors propose a pathogenetic process of chronic subdural hematoma : 1) Development of posttraumatic subdural hygroma, not encapsulated, 2) hemorrhage and subdural clot-formation at a later date, which develops into 3) an expanding, encapsulated subdural hematoma, in a subacute cours. of 2-3 weeks.
Copyright © 1979, Igaku-Shoin Ltd. All rights reserved.


