Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
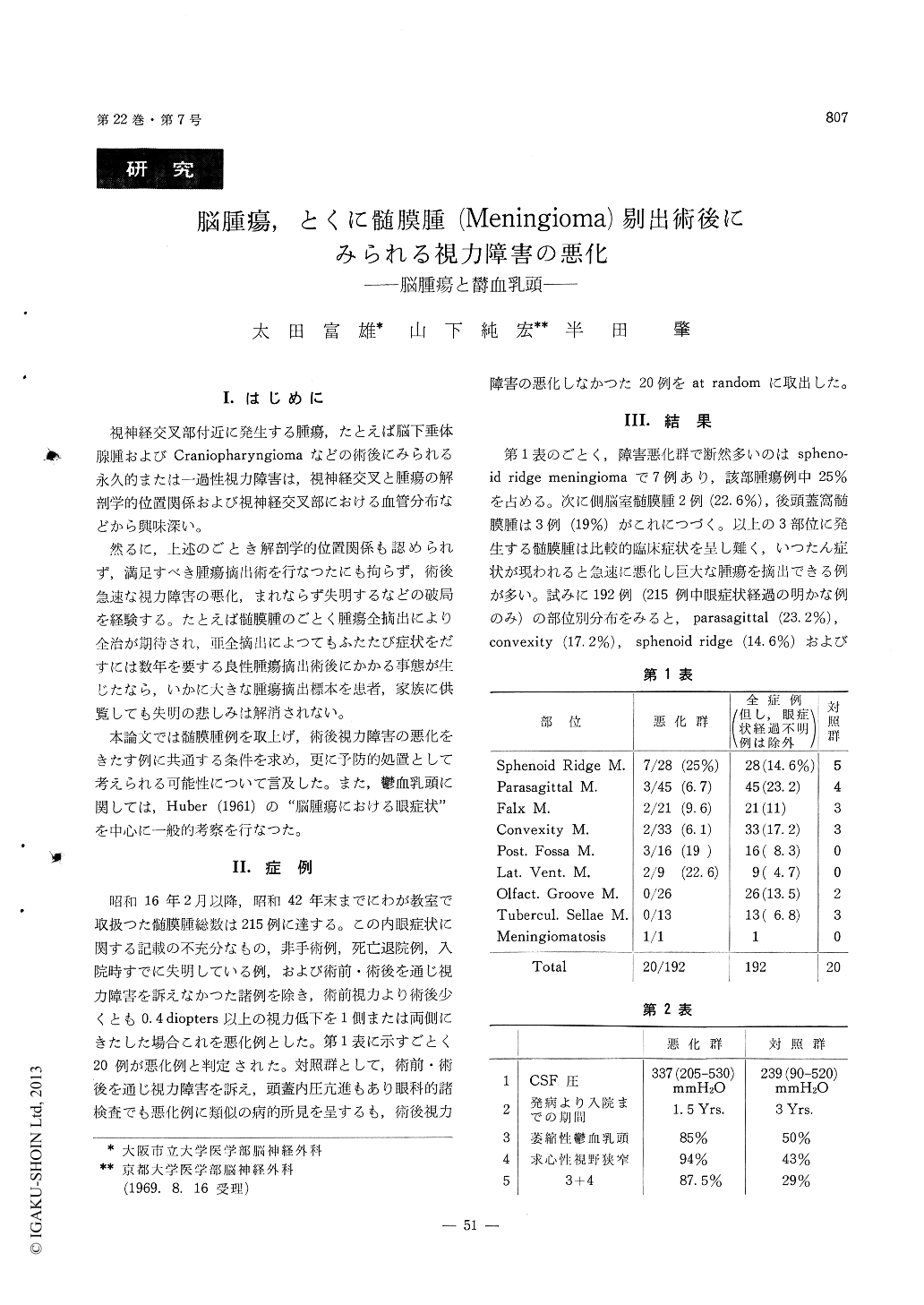
1)昭和16年2月以降42年末までに,われわれの教室で取扱つた髄膜腫患者は215例に達する。そのうち,術後視力障害が増悪(0.4diopters以上の視力低下または失明)したのは20例あつた。
2)視力障害悪化例20例について調査した結果,(a)発生部位は蝶形骨稜,側脳室および後頭蓋窩のごとく,比較的後期まで症状を現わし難い部分に多い。(b)発病より入院までの期間は平均18カ月で,対照群の平均35カ月の約半分である。すなわち,末期まで症状を出さずいつたん発病すれば急速に悪化する。換言すればmaxi−rnumに適応してきた頭蓋内環境がある時期に達すれば急速にくずれ去ることを意味している。(c)髄液圧平均は337mmH2Oで,対照群の239mmH2Oより著明に高い。(d)萎縮性轡血乳頭は1例を除き検査され得た全例に認められた(85%)。対照群では50%に認められた。求心性視野狭窄は93%に認められ,対照群の43%に比しはるかに高率を示す,萎縮性轡血乳頭と求心性視野狭窄の合併は87%にみられ,対照群の29%より著明に高率であつた。
3)以上のことより結論されることは,髄膜腫のごとき良性腫瘍が比較的症状を示し難い部位に発生した場合,視力障害を主訴として入院するものが多く,萎縮性轡血乳頭とその結果として起る求心性視野狭窄の認められる例では,たとえ腫瘍の全摘出を試みても視力障害の改善よりむしろ悪化する例が圧到的に多い。
4)かかる破局を避ける手段は現在なく,われわれはかかる例を緊急例として先ず非観血的減圧操作(尿素,マニトール)を試み,更に腫瘍摘出術も極力侵襲の少い方法で行われるべきことを提案する。必要な際には手術を数回に分け,視力障害の推移をみるのも良策と思う。
5)Huber,A.(1961)の著書,"Eye Symptoms inBrain Tumors"を参考にし鬱血乳頭全般について考察を加えた。
Two hundred and fifteen cases of meningiomas in different locations have been experienced in our de-partment since February, 1941 up to the end of 1967. Among them, postoperative deterioration of the visual disturbance, that is, visual loss beyond 0.4 diopters comparing to preoperative visual acuity or total blindness has been recorded in 20 cases.
Analysing these 20 cases, the following results have been obtained : ( 1 ) Tumor have been apt to be located in the areas where symptoms are difficult to reveal until the late stage, such as around the sphenoid ridge, in the lateral ventricle or in the infratentorial space. ( 2 ) Patients have been admit-ted in 18 months in average after the appearance of symptoms, comparing to 35 months in average in the control group. Such a rapid aggravation, once it occurs, might mean that intracranial circum-stances adapted in maximum rapidly fall into the earth as soon as somethings are added to them. ( 3 ) Average CSF pressure have been 337 mmH2O and remarkably higher than 239 mmH2O in the control group. ( 4 ) Papilledema in an atrophic stage has been demonstrated in all examined cases except for one (85%), while it has been demon-strated in 50% of the control group. Concentrated narrowing of the visual field has been revealed in 93% remarkably higher than 43% of the controlgroup. Combination of papilledema in an atrophic stage and concentrated narrowing of the visual field has been obtained in 87% comparing to 27% in the control group.
According to these resulft it could be concluded that, in case there is a combination of papilledema in an atrophic stage and concentrated narrowing of the visual field, there are remarkably high inci-dence in which visual disturbance is deteriorated rather than being improved even if the tumor is totally extirpated. None of the procedures, so far, has been effective to avoid such a catastrophe.However, we reasonably propose to treat them in emergency, to try non-operative reduction of increa-sed intracranial pressure with different dehydrators, and then to consider operative procedures in a mini-mum extent. If necessary, removal of the tumor can be divided into several times so as to be able to follow up the course of the visual acuity in each of operative procedures.
General views of the papilledema have been dis-cussed in accordance with Huber's "Eye Symptoms in Brain Tumors" (1961).
Copyright © 1970, Igaku-Shoin Ltd. All rights reserved.


