Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
くも膜下出血の原因は,その大部分が脳動脈瘤の破裂によるものであり,その動脈瘤症例に対する手術療法と姑息的療法との成績の比較では明らかに前者が良好であり,脳動脈瘤は手術すべきものであるということはしだいに常識化されつつある。また,脳動脈瘤に対する手術方法としては頸部頸動脈の結紮手術,開頭による動脈瘤への直接手術におよそ大別することができるが,ある部位のものを除けば直接手術の方が確実であり成績もよい。
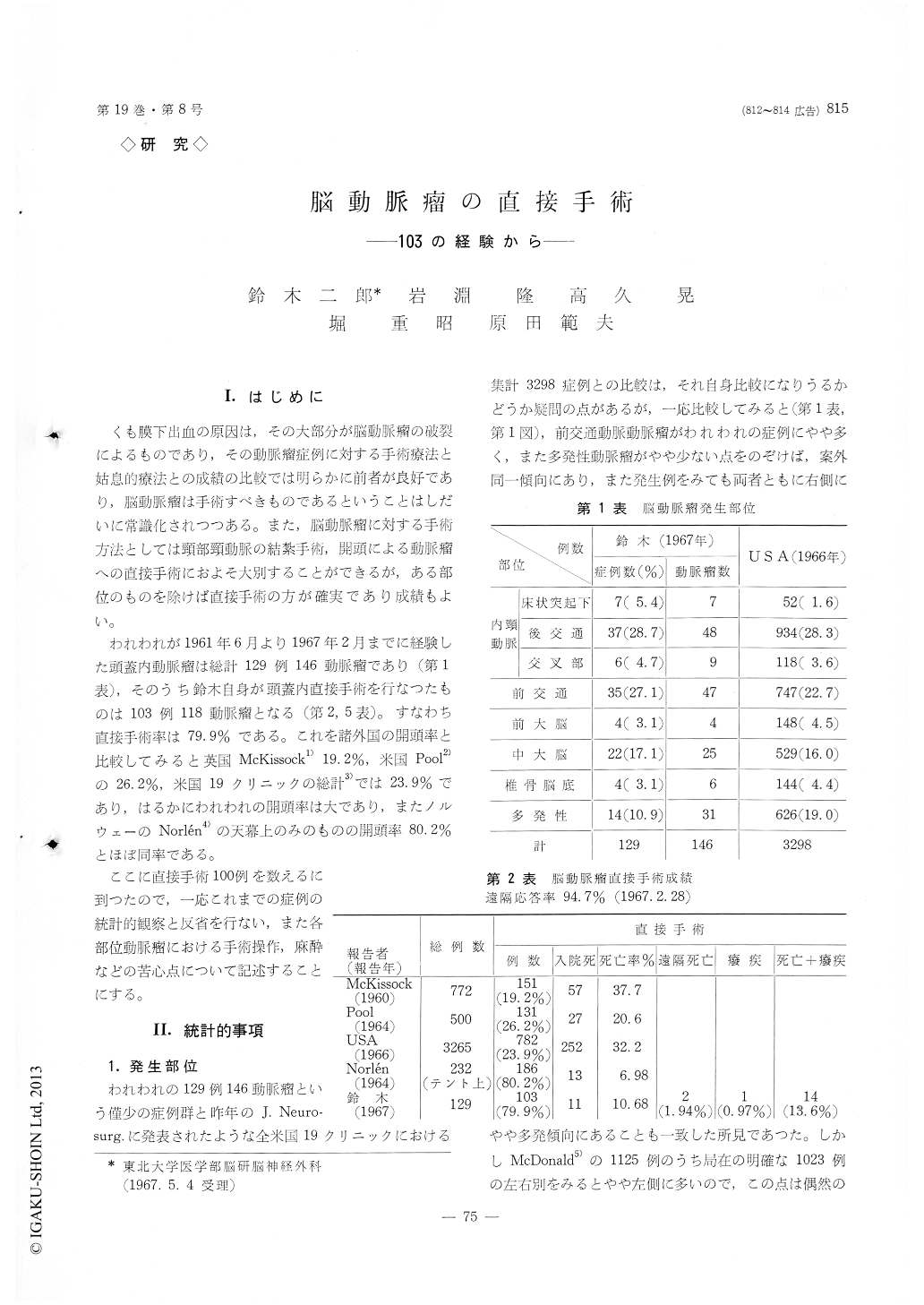
われわれが1961年6月より1967年2月までに経験した頭蓋内動脈瘤は総計129例146動脈瘤であり(第1表),そのうち鈴木自身が頭蓋内直接手術を行なつたものは103例118動脈瘤となる(第2,5表)。すなわち直接手術率は79.9%である。これを諸外国の開頭率と比較してみると英国McKissock1)19.2%,米国Pool2)の26.2%,米国19クリニックの総計3)では23.9%であり,はるかにわれわれの開頭率は大であり,またノルウェーのNorlen4)の天幕上のみのものの開頭率80.2%とほぼ同率である。
This review is based upon 103 cases with the intracranial aneurysms directly attacked by the authors upon between June 1961 and February 1967.
Ninety cases of these had single aneurysm, 10 cases two aneurysms, and 3 cases three aneurysms.
As the total of 129 cases of intracranial aneurysms (149 aneurysms) have been experienced during this period at the authors' clinic, the ratio of direct oper-ation was 79. 9% of the total cases.
The satisfactory or suitable procedures, ligation or clipping of the neck of aneurysms, were performed on 100 cases, and the unsatisfactory or unsuitable procedures, coating or wrapping of aneurysm, on the rest of the cases.
Seventy-seven cases of them were the favorable risk patients, and the rest of them were the poor risk patients. Five cases of the former group patients, and 6 cases of the later group came to autopsy.
As the result, mortality rate was 10. 68%.
According to the follow-up study after discharge from the hospital, 2 cases died, 1 case was morbid, and the others were healthy or possible to walk by themselves at least.
The technical specialities in direct attack of intracra-nial aneurysms were given below for each localization of aneurysms.
For the aneuysm arising from the junction of the internal carotid and the posterior communicating artery, the neck of the aneurysm is approached through the authors' method, temporal keel form incision, which is much more beneficial and safer than the traditional approach.
There are some types of the aneurysm in such a place as follows, which must be paid special attention for clipping.
1) the aneurysm with atheroma plaque in the neck, which may occlude or narrow the lumen of the carotid artery as the result of clipping.
2) one with severe arteriosclerosis in the wall of the internal carotid artery and the wall of aneurysm, which may occlude or narrow the lumen of the in-ternal carotid artery as the result of clipping or liga-tion.
3) the bubble- like small aneurysm bordering the main aneurysm, which may rupture by the procedure of clipping or ligation.
4) the anterior choroidal artery, which is behind the neck of the aneurysm and unawared, may be occluded togather by clipping.
5) the broader neck more than 10 mm in diameter, which may narrow the lumen of the internal carotid artery by clipping, but the cases without sclerosis and atheroma in the neck are possible to be ligated. The aneurysm of the anterior communicating artery is always approached through the bifrontal incision. Before exposing the neck of aneurysm, the anterior cerebral arteries must be exposed from the fork of the internal carotid artery for temporary clipping.
Even in aneurysm as large as more than 15mm in diameter, at such location, occlusion of the neck is possible by clipping after ligation of the neck.
Of course, the growth direction of the aneurysm, the grade of adhesion with four export and import arteries, the size of aneurysm, and the deformity of the anterior communicating artery may have influence upon the difficulty of this procedure.
Anyhow, certification of the four export and import arteries, and preparation of them from aneurysm it-self are the fundamental point of this operation. Three of 39 cases with the anterior communicating artery aneurysm came to autopsy, making the mortal-ity rate 7.7%.
In the authors' opinion, experiencing four basilar artery aneurysms, the approach through the contrala-teral side of the growth direction of the aneurysm is preferable for neck-clipping at such location, although bilateral occulomotor nerves and the tentorial notch may interfere considerably with approach to the neck. The aneurysm more than 15mm in diameter at suchlocation may not be able to be attacked at its neck, because the operator can not verify the feeding arteries of the aneurysm due to the large aneurysm itself which fills the bottom of the operative field.
There have been some discussions on the treatment of the multiple intracranial aneurysms, while someone asserted that treatment of the ruptured aneurysm only was enough, but the others emphasized that all of the aneurysms including ruptured had to be treated.
Judging from our knowledge, the latter opinion is adoptable, because the operative procedure only for the ruptured aneurysm will provoke rupture of the other aneurysms due to the change of intracranial hemo-dynamics.
From these reasons, direct operation with a single skin incision and craniotomy is desirable, through which every aneurysm can be treated at the same time. And authors have disigned several new skin incisions and craniotomies for this procedure, consid-ering various combinations of the aneurysmal distribu-tion.
Hypothermic anesthesia ranging from 23℃ to 29℃ were adopted in all cases. Cardiac arrest occurred'in 3 cases as the complication of hypothermic anesthesia, but all of them could be resuscitated and are healthy now.
The approval time of temporary occlusion of the various feeding arteries under hypothermic anesthesia was discussed. The conclusion was that the body tem-perature should not be dropped lower than 25℃, and that the approval time of temporary occlusion for every feeding arteries at 26℃ was about 60 minutes in total, devided in three times. The operative procedure of placing a suture around the intracranial artery is of-ten very difficult. The procedure would be easier if a simpler and surer method could be found to guide the suture around the artery or the neck of the an-eurysm.
The authors have designed a magnetic instrument for this purpose.
Copyright © 1967, Igaku-Shoin Ltd. All rights reserved.


