Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
難治性心不全例に対する血管拡張薬の応用—vaso—dilator therapyは,心臓全体としての前負荷,後負荷,あるいはその両者を減じて肺うっ血を軽減し,心拍出量増加の可能性を生じ,臨床症状の改善をきたすとされる1〜3)。しかし,右室を中心に考え,肺高血圧症,特に前毛細管性肺高血圧症とそれに伴う右室機能異常に本治療法がどのように作用するかを充分に検討した報告はない。
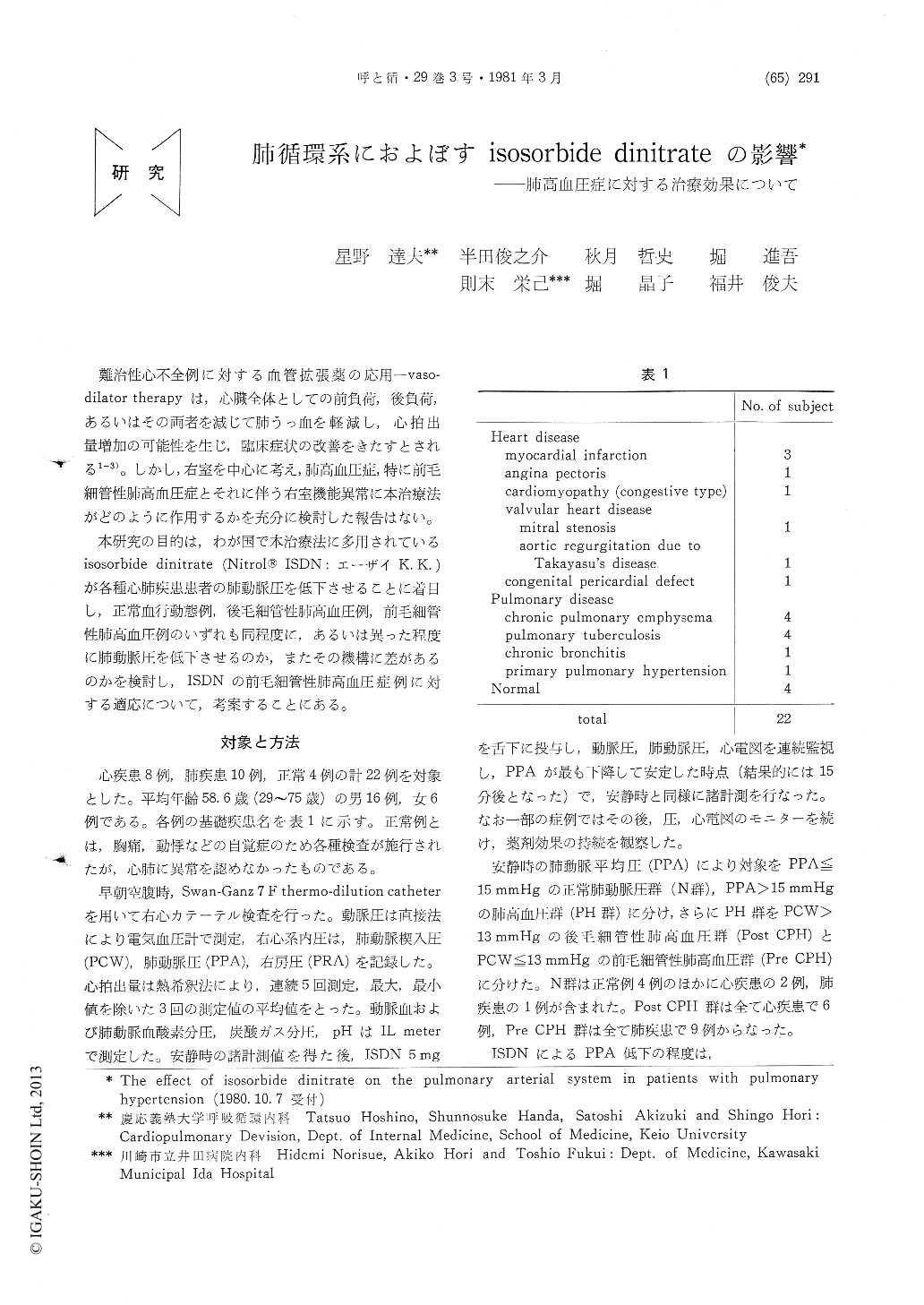
本研究の目的は,わが国で本治療法に多用されているisosorbide dinitrate (Nitrol®ISDN:エーザイK. K.)が各種心肺疾患患者の肺動脈圧を低下させることに着目し,正常血行動態例,後毛細管性肺高血圧例,前毛細管性肺高血圧例のいずれも同程度に,あるいは異った程度に肺動脈圧を低下させるのか,またその機構に差があるのかを検討し,ISDNの前毛細管性肺高血圧症例に対する適応について,考案することにある。
The effect of isosorbide dinitrate (ISDN) on the pulmonary arterial system was evaluated with cardiac catheterization in 8 patients with heart diseases, 10 with chronic pulmonary diseases and 4 subjects without cardiopulmonary disease. Fif-teen of 22 patients had pulmonary hypertension (PH), with mean pulmonary arterial pressure be-tween 17 mmHg and 42 mmHg. They included 9 patients with precapillary and 6 patients with postcapillary PH. Pressures in right atrium, pul-monary artery and pulmonary capillary wedge position and pulmonary blood flow (PBF) were measured. Pulmonary arteriolar resistance (PAR), pulmonary arterial compliance (PAC) and pulmo-nary artery time constant were calculated, based of the alternating current theory by Engelberg and DuBois. Five mg of sublingual ISDN were given and 15 min later with maximum effect on hemodynamics, recording were repeated. The pressures were decreased significantly. The mean pulmonary arterial pressure in patients with PH decreased more than it in patients without PH. PBF in patients without PH was reduced, though it in patients with PH did not change. Accord-ingly, PAR was decreased in patients with PH, while did not change in those without PH. In patients with chronic pulmonary disease, arterial hypoxia did not change. We concluded, ISDN was useful for the treatment of precapillary and postcapillary PH. Right ventricular afterload decreased, as well as preload. In patients with low preload, however, ISDN might develop sys-temic hypotension as an adverse reaction. The change in PAR suggested active change in tone of the muscular pulmonary arteries, though the decrease in PAC was passive and related with decrease in pulmonary arterial pressure.
Copyright © 1981, Igaku-Shoin Ltd. All rights reserved.


