Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
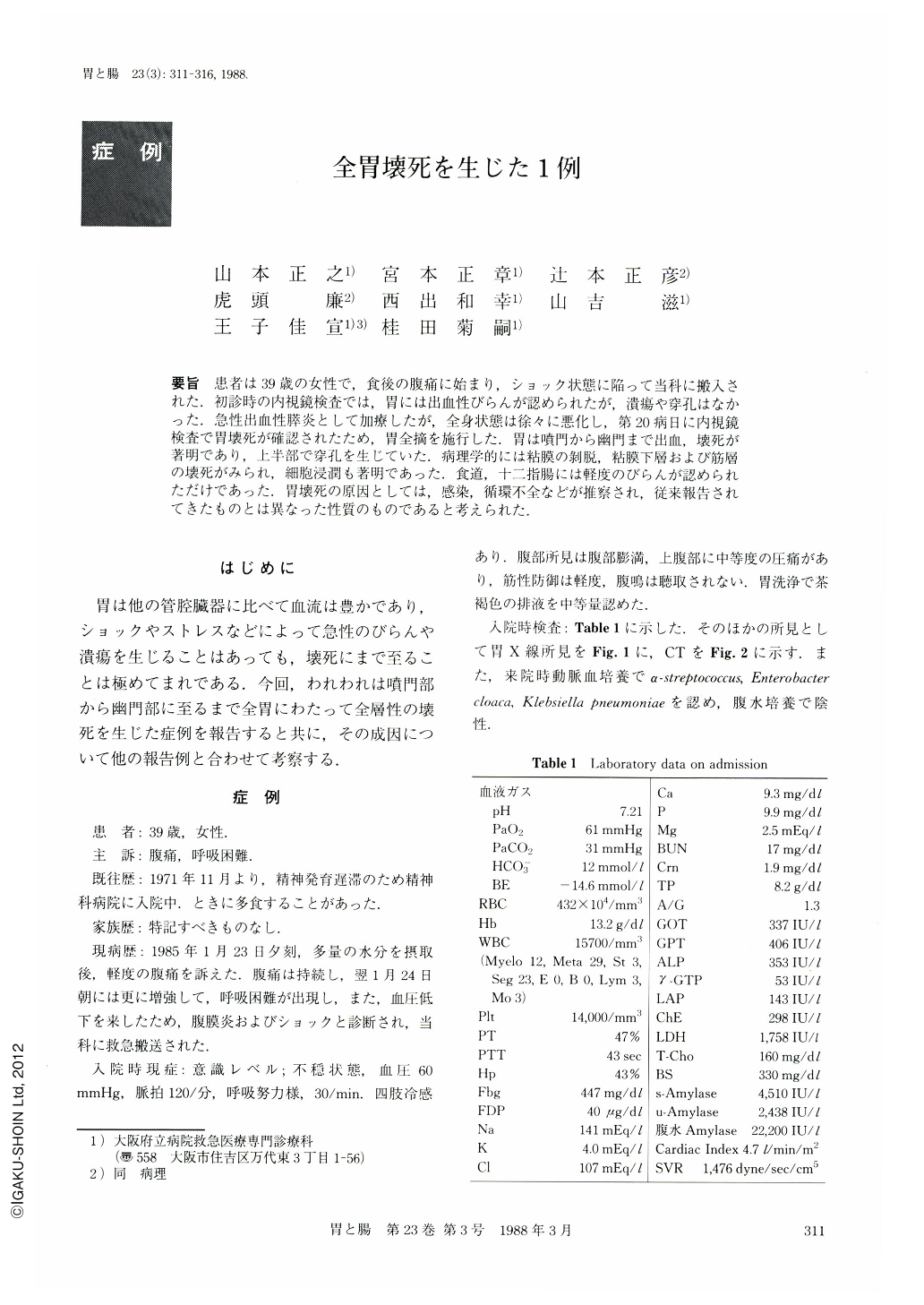
要旨 患者は39歳の女性で,食後の腹痛に始まり,ショック状態に陥って当科に搬入された.初診時の内視鏡検査では,胃には出血性びらんが認められたが,潰瘍や穿孔はなかった.急性出血性膵炎として加療したが,全身状態は徐々に悪化し,第20病日に内視鏡検査で胃壊死が確認されたため,胃全摘を施行した.胃は噴門から幽門まで出血,壊死が著明であり,上半部で穿孔を生じていた.病理学的には粘膜の剝脱,粘膜下層および筋層の壊死がみられ,細胞浸潤も著明であった.食道,十二指腸には軽度のびらんが認められただけであった.胃壊死の原因としては,感染,循環不全などが推察され,従来報告されてきたものとは異なった性質のものであると考えられた.
A 39 year-old woman who camplained of upper abdominal pain after a meal was admitted in a state of shock to our emergency department. She was diagnosed and treated as having acute hemorrhagic pancreatitis. On the 21st day after hospitalization, her general condition had deteriorated because of sepsis, and gastric necrosis with perforation was found. Total gastrectomy was performed. No lesion was found in the esophagus nor the duodenum at operation.
The entire resected stomach showed severe hemorrhagic necrosis and sloughing of the entire mucosa with a perforation of its upper part. Microscopic examination revealed full thickness necrosis of the gastric wall with marked round cell infiltration. There was no microabscesses. These histologic features were quite different from classical phlegmonous gastritis. The exact cause of gastric necrosis was unknown, but systemic infection and focal hypoperfusion was considered to be a major aggravating factor.
Copyright © 1988, Igaku-Shoin Ltd. All rights reserved.


