Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
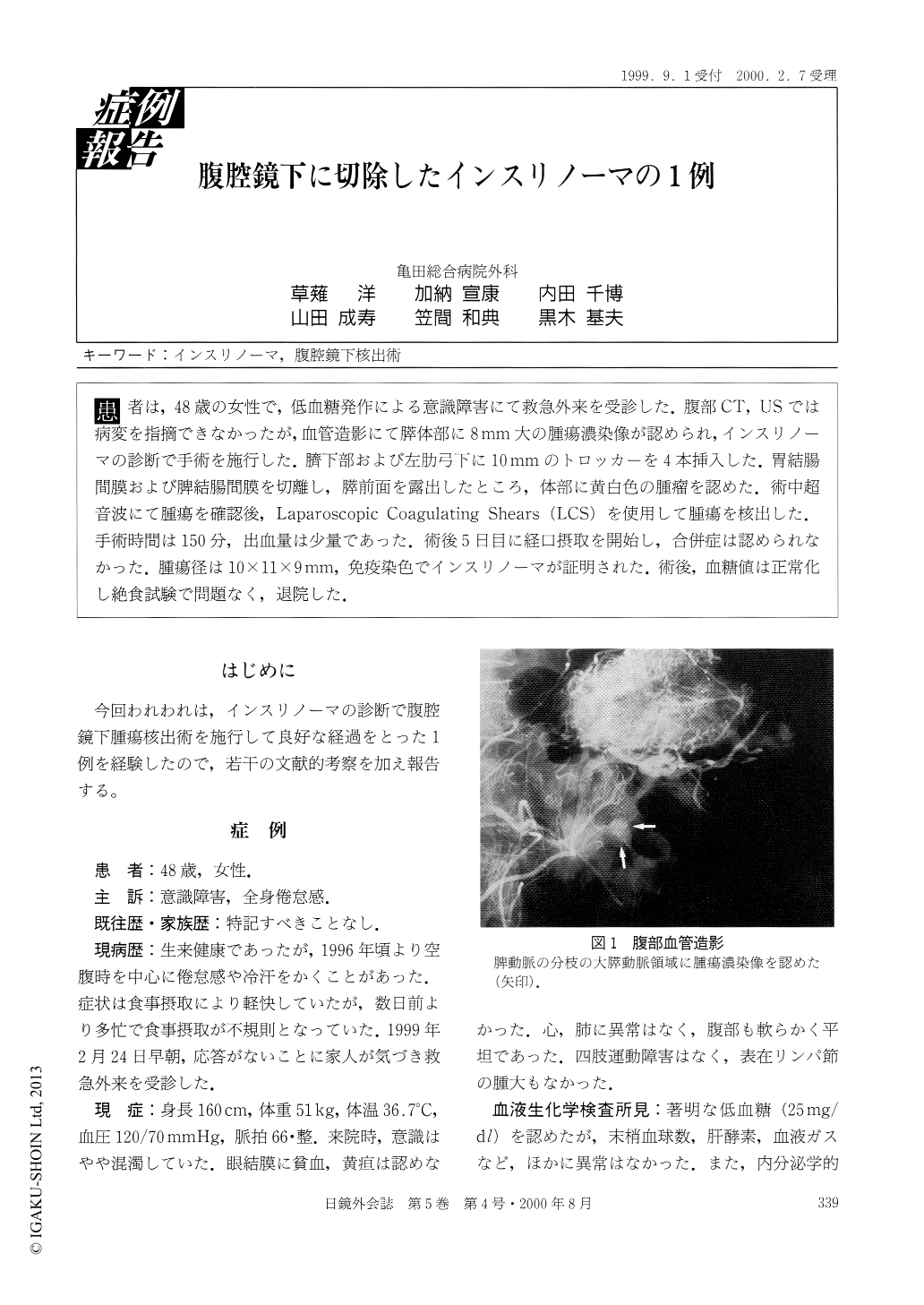
患者は,48歳の女性で,低血糖発作による意識障害にて救急外来を受診した.腹部CT, USでは病変を指摘できなかったが,血管造影にて膵体部に8mm大の腫瘍濃染像が認められ,インスリノーマの診断で手術を施行した.膀下部および左肋弓下に10mmのトロッカーを4本挿入した.胃結腸間膜および脾結腸間膜を切離し,膵前面を露出したところ,体部に黄白色の腫瘤を認めた.術中超音波にて腫瘍を確認後,Laparoscopic Coagulating Shears(LCS)を使用して腫瘍を核出した.手術時間は150分,出血量は少量であった.術後5日目に経口摂取を開始し,合併症は認められなかった.腫瘍径は10×11×9mm,免疫染色でインスリノーマが証明された.術後,血糖値は正常化し絶食試験で問題なく,退院した.
A 48-year-old women was admitted to the hospital because of consciousness disturbance due to hypog-lycemia. No tumor was detected by abdominal ultrasonography or enhanced CT scan. A celiac angiogram showed a tumor stain, 8 mm in diameter, in pancreatic body. A diagnosis of a solitary pancreatic insulinoma was confirmed and laparoscopic enucleation of the tumor was perfomed. Access was gained via four laparoscopic cannulae positioned arouned the upper abdomen. The gastrocolic omentum was opened widely and pancreas was displayed by lifting the stomach. The insulinoma was localized in pancreatic body.
Copyright © 2000, JAPAN SOCIETY FOR ENDOSCOPIC SURGERY All rights reserved.