Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- 参考文献 Reference
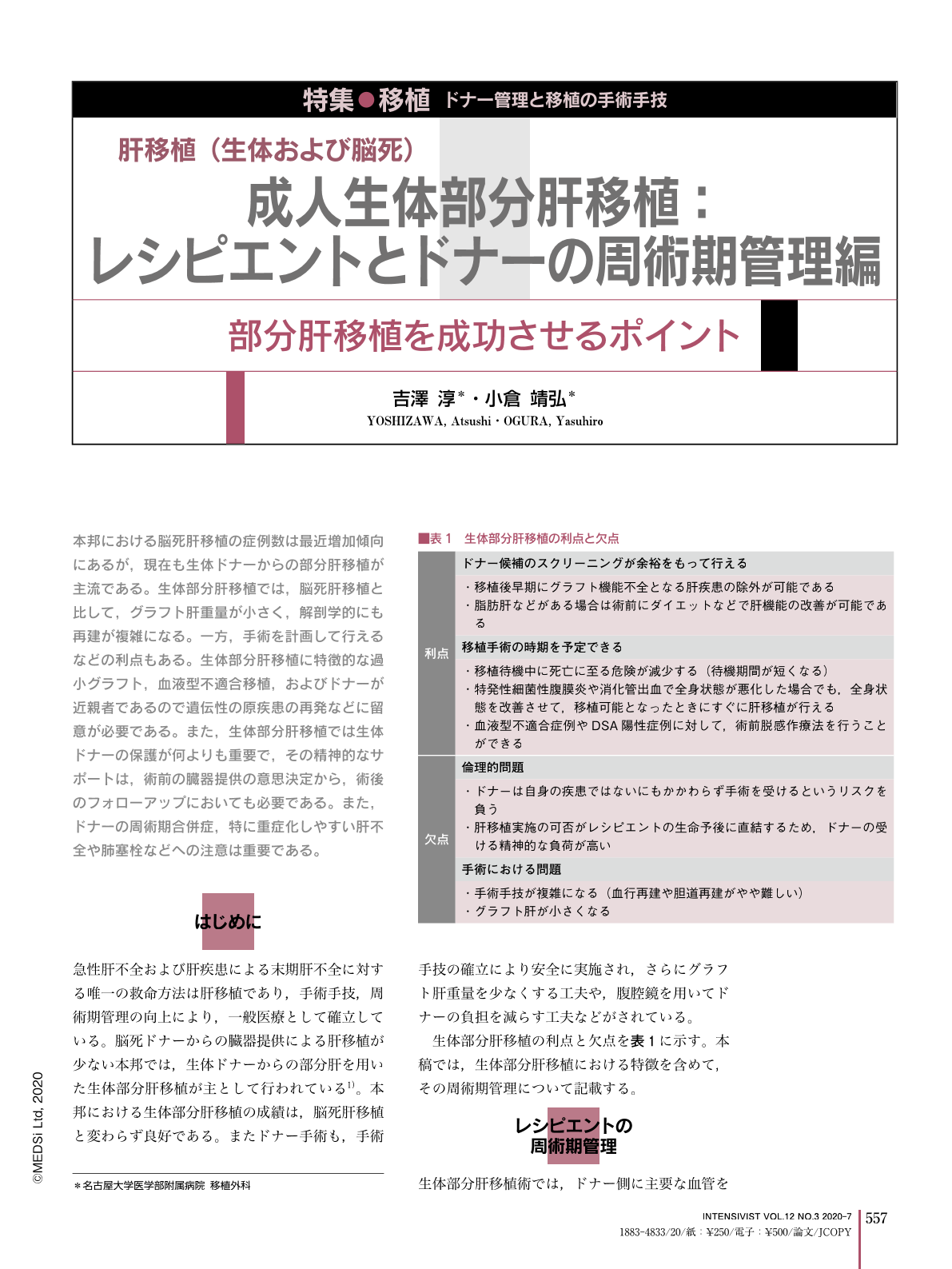
本邦における脳死肝移植の症例数は最近増加傾向にあるが,現在も生体ドナーからの部分肝移植が主流である。生体部分肝移植では,脳死肝移植と比して,グラフト肝重量が小さく,解剖学的にも再建が複雑になる。一方,手術を計画して行えるなどの利点もある。生体部分肝移植に特徴的な過小グラフト,血液型不適合移植,およびドナーが近親者であるので遺伝性の原疾患の再発などに留意が必要である。また,生体部分肝移植では生体ドナーの保護が何よりも重要で,その精神的なサポートは,術前の臓器提供の意思決定から,術後のフォローアップにおいても必要である。また,ドナーの周術期合併症,特に重症化しやすい肝不全や肺塞栓などへの注意は重要である。
Living donor liver transplantation (LDLT) is prevalent in Japan because of the organ shortage, although the number of deceased donor liver transplants is increasing. The outcome of adult LDLT has improved. There are some issues specific to LDLT, such as a small-for-size grafts, ABO-incompatibility, pre-sensitized donors, and so on. One of the most important issues is donor safety, including donor selection, peri-operative management and long-term outcomes. One of the most important points for donor selection is to confirm an independent will to donate without any obligation, including a psychosocial evaluation. Medical evaluation is also important, including medical examination, history, and the absence of steatosis. Imaging evaluation for volumetry and surgical anatomy is used for graft-type selection and to rule-out steatosis. There should be special consideration for the patients with inherited liver diseases. Fatal complications such as liver failure and pulmonary embolism must be avoided in the perioperative management after the donor operation. There are complications possible after the donor operation such as bile leakage, ileus, and incisional hernia. We also should care for the psychological health of the donors. In some cases, liaison psychiatry is helpful for mental support for the living donors.
Copyright © 2020, MEDICAL SCIENCES INTERNATIONAL, LTD. All rights reserved.


