Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
はじめに
椎間板は,中央部の髄核(nucleus pulposus)と周辺部の線維輪(annulus fibrosus)からなり,椎間板の上下面は軟骨板(cartilage end-plate)にて椎体と強く付着する。線維輪は内層と外層(Sharpey線維)からなる。
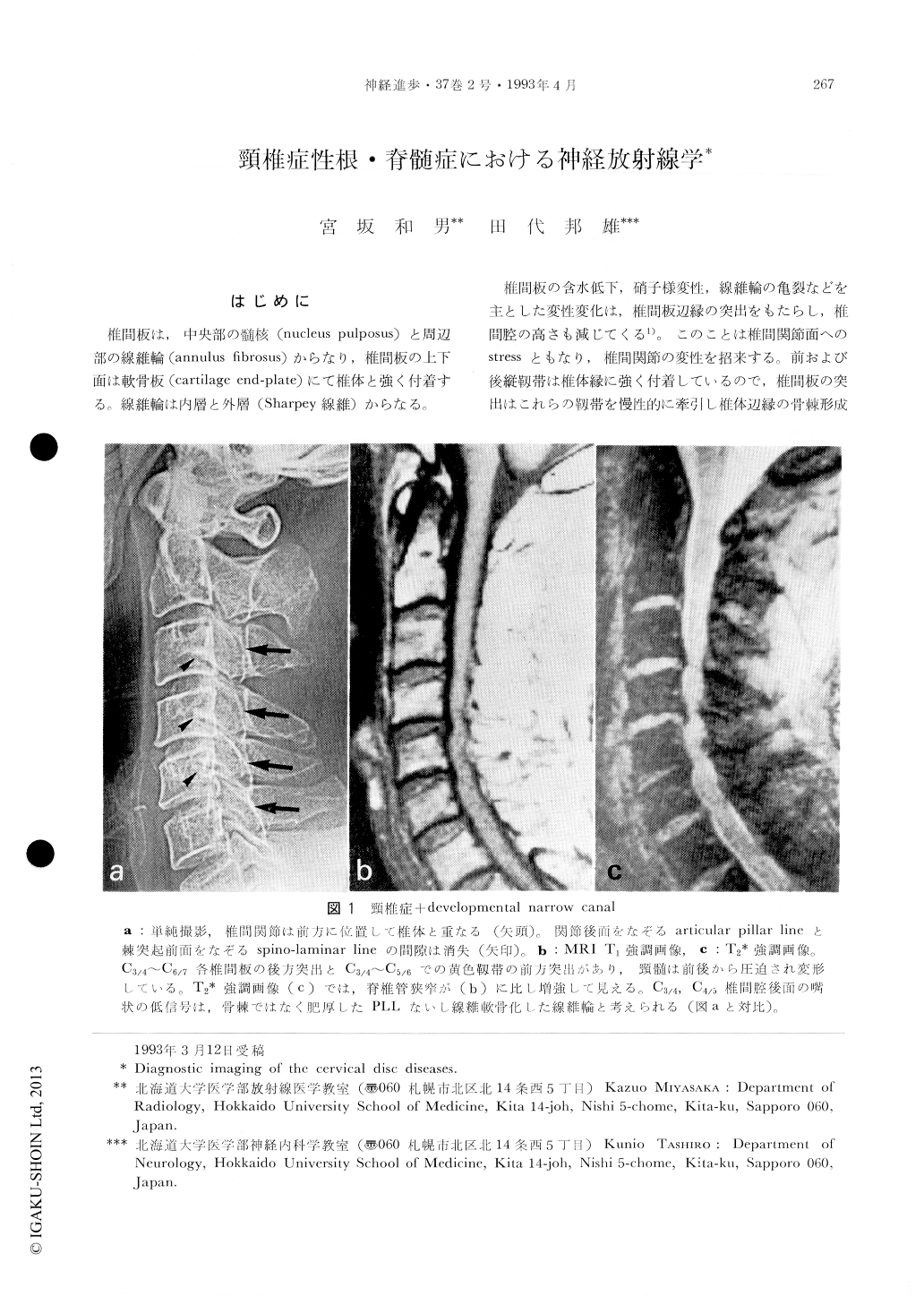
椎間板の含水低下,硝子様変性,線維輪の亀裂などを主とした変性変化は,椎間板辺縁の突出をもたらし,椎間腔の高さも減じてくる1)。このことは椎間関節面へのstressともなり,椎間関節の変性を招来する。前および後縦靱帯は椎体縁に強く付着しているので,椎間板の突出はこれらの靱帯を慢性的に牽引し椎体辺縁の骨棘形成に至る。頸樵では鉤椎関節(Luschka関節)にもstressとなり,同関節の肥厚・骨棘を生ずる。いわゆるspondylosisである。このような椎間板および関節の変性は悪循環であり,加えて黄色靱帯の肥厚ないしはたわみ込み(infolding),亜脱臼を伴い,脊椎管狭窄を増長する。椎間板変性の過程でなんらかの強い外力が加わると,椎間板髄核が線維輪の亀裂を貫通して脱出する。いわゆる椎間板ヘルニア(髄核ヘルニア)である.高齢者の椎間板には線維輪亀裂が頻発するが,髄核自体も軟らかなゲル様構造を失うために,かえって髄核ヘルニアは減少する。
Many imaging modalities are currently available for the diagnosis of the cervical disc diseases. Myelography has been the examination of choice in cervical disc diseases for a long time, especially using non-ionic water soluble contrast agent. With the advent of high resolution CT, coupled with or without contrast material, the diagnostic accuracy has been greatly improved. Furthermore, recent revolution of MRI with a high-field magnet, highly sensitive coil and motion suppression technique has given great advantages for the evaluation of the disc diseases.
What is important in evaluating the cervical disc diseases is; first, to delineate disc protrusion and osteophyte suitably; second, to understand the associated findings with disc diseases including congenital or developmental narrow canal, OPLL, subluxation and dynamic changes of cervical spine on neck flexion and extension, and intramedullary changes secondary to extrinsic spinal cord compression; and third, to correlate the image findings to neurological sign. Identification of protruded disc and osteophyte is directly made by CT and MRI. On T1 weighted image herniated disc is seen as intermediated signal intensity while on T2 weighted image it is high signal intensity. In the patient with myelopathy and radiculomyelopathy MRI is superior to CT since MRI dipicts disc material and its location, deformity of the spinal cord, intramedullary change within the material and its location, dynamic change of the cervical spine non-invasively. However, MRI is not always better than CT in evaluating patients with radiculopathy. It is especially ture in the cases with bony changes such as osteophyte, OPLL and narrow canal. Some disc materials above C6 level may be better appreciated by CT. When there are spondylotic changes at multiple levels and a responsible lesion for the patient symptoms is not conclusive, myelographic study will be performed, and followed by CT myelography.
Copyright © 1993, Igaku-Shoin Ltd. All rights reserved.


