Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
抄録 原因不明のショックを数回繰り返し,頭部CT上,両側対称性に大脳基底核に出血性梗塞像を呈し,臨床的には錐体路症状から錐体外路症状への移行がみられたが症状の改善なく,79日目に死亡した症例である。神経病理学的には,病巣分布はScholzらのいうanoxiaに対する選択的易損性の部位に一致し,ショックが重なったため病巣が拡がったものと考察した。また本例では,anoxiaで壊死をきたすのは珍しいとされる黒質網状帯が両側性に壊死に陥っており,特筆された。anoxiaによる脳障害の報告は多いが,本例のように両側対称性に尾状核,被殻,淡蒼球に壊死をきたした症例はまれと思われる。
We reported a case with bilateral necrosis of the basal ganglia after hypotensive shocks. The patient was a 69-year-old woman, who fell into a hypotensive shock (B. P. below 40 mmHg) of unknown origin during examination of her blad-der cancer and was admitted into CCU.
After admission, hypotensive shocks were repeat-ed four times (B. P. below 50 mmHg each time).Neurological examination revealed a left spastic hemiplegia. Brain CT on 10 th day showed bi-laterally low density areas around the basal ganglia and a diagnosis of brain infarction was made.
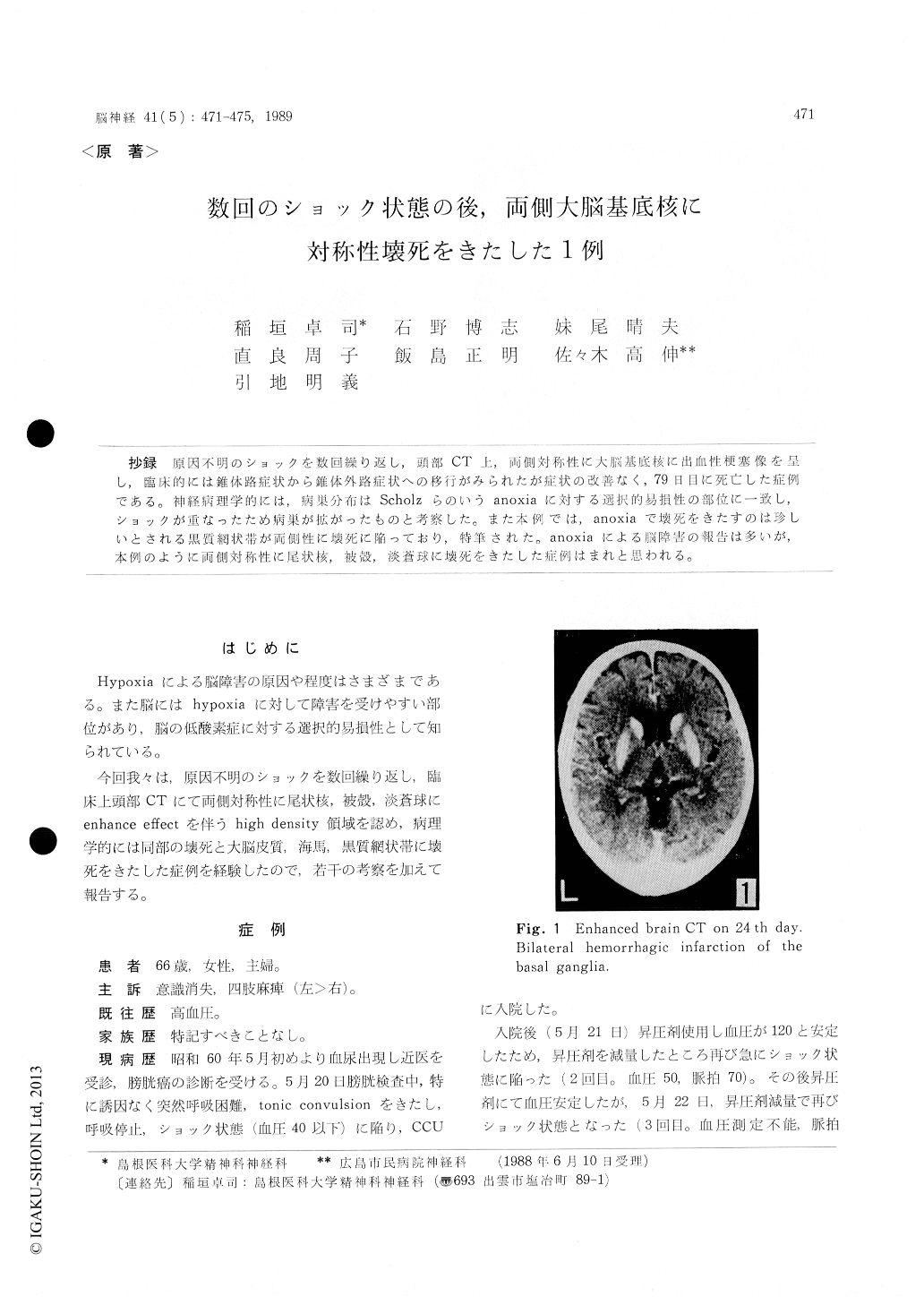
She gradually presented quadriplegia and sym-ptomatic changes from pyramidal to extrapyrami-dal signs. Brain CT on 24 th day showed bilate-ral hemorrhagic infarction of the basal ganglia with enhanced effect. On 79 th day, she again fell into shock and died.
Neuropathological examination of the brain was as follows. 1) laminar necrosis of the deep layers of the cerebral cortex, 2) bilateral necrosis of the hippocampal Sommer sector, 3) bilateral nec-rosis of the caudate nucleus, putamen and pal-lidum with neuronal loss and infiltration of fat granule cells, 4) sparing of the internal capsules, 5) bilateral necrosis of the reticular zone of the substantia nigra, 6) foci of fresh necrosis and loss of Purkinje cells in the cerebellum. These lesions are consistent with those of selective vulnerability in hypoxia as described by Scholz et al.
An extensive distribution of cerebral as well as basal ganglia necrosis in this case was caused by repeated shocks. A special mention was made on bilateral necrosis of the reticular zone of the substantia nigra in this case, because a survey of the literature shows that necrosis of this re-gion has been rarely reported neuropathologically.
Copyright © 1989, Igaku-Shoin Ltd. All rights reserved.


