Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
癌特異抗原の検索に対する研究11,17,18)が近年めざましい進歩をとげているが,一方では発癌過程,担癌状態における免疫学的機構の解析にも多くの注目が集められている1,15,20,23)。これまでの知見によれば,担癌体では,その進展とともに主として細胞性免疫能の低下が指摘されてきたが9,21),その積極的な証明は近年に至るまでなされなかつたと言える1,6,8,23)。一方,免疫現象の主役としてリンパ球に対する関心が高まるにつれ,それが発生由来および機能の上からも単一のPopulationではないことが明らかにされた13〜15)。即ち,いわゆる胸腺由来リンパ球(以下T-cellと略す)と骨髄由来リンパ球(以下B-cellと略す)がそれであり,発生由来から命名されたこれら2種類のリンパ球も,機能面では前者は遅延型過敏反応,移植免疫,ウィルス感染防禦等,いわゆる細胞性免疫に関係し,後者は抗体産生細胞であるプラズマ細胞の前駆細胞として抗体(Ig)産生に関与していると言われている7,25〜27)。最近種々の疾患における生体の免疫応答をこれらリンパ球との関連において観察した報告も数多くみられるようになつてきたが,今後リンパ球機能がその分化の過程の中でさらに細かく位置づけられれば,生体の防禦機構としての免疫応答も一層明確なものになるにちがいない。
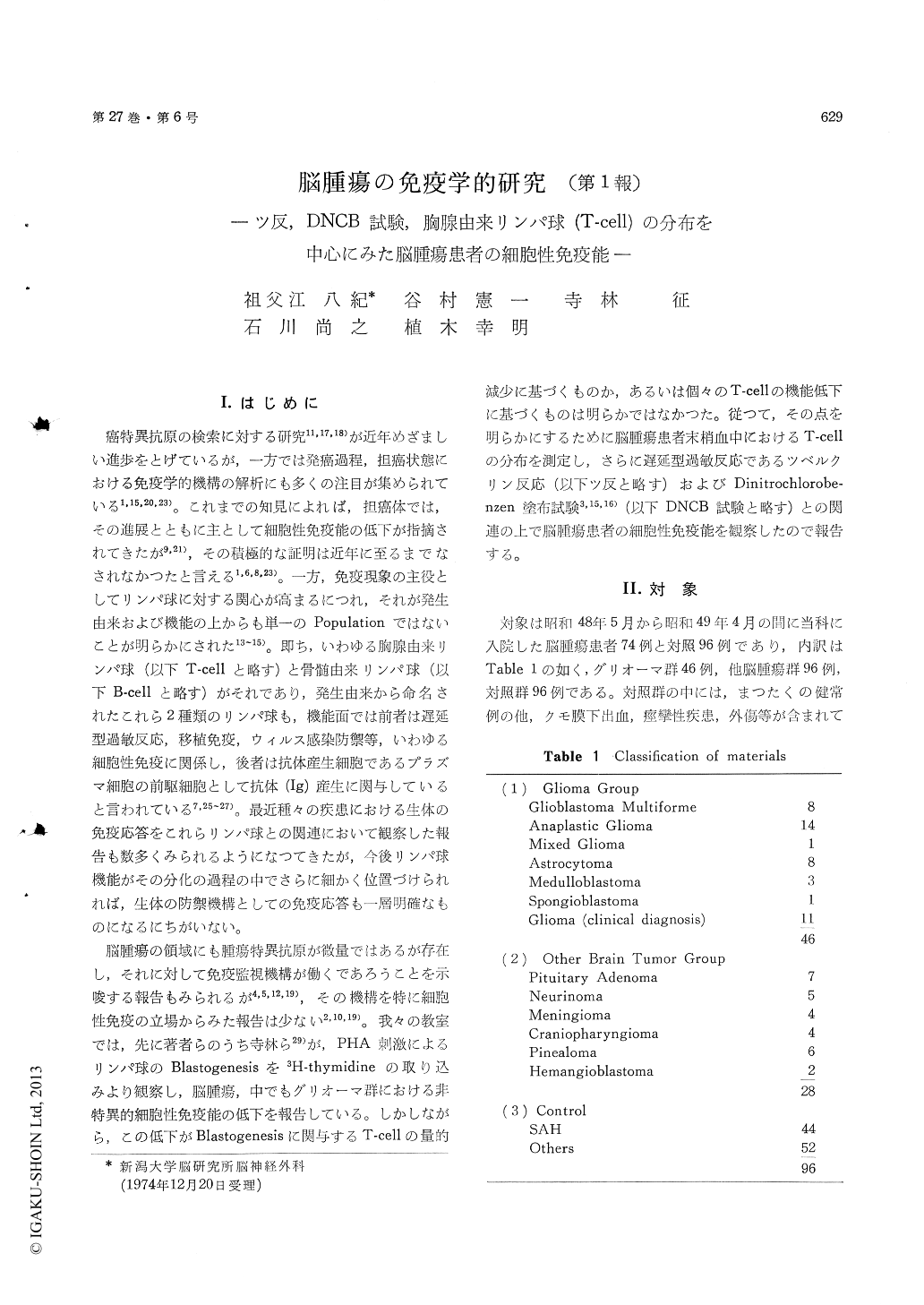
脳腫瘍の領域にも腫瘍特異抗原が微量ではあるが存在し,それに対して免疫監視機構が働くであろうことを示唆する報告もみられるが4,5,12,19),その機構を特に細胞性免疫の立場からみた報告は少ない2,10,19)。我々の教室では,先に著者らのうち寺林ら29)が,PHA刺激によるリンパ球のBlastogenesisを3H-thymidineの取り込みより観察し,脳腫瘍,中でもグリオーマ群における非特異的細胞性免疫能の低下を報告している。しかしながら,この低下がBlastogenesisに関与するT-cellの量的減少に基づくものか,あるいは個々のT-cellの機能低下に基づくものは明らかではなかつた。従つて,その点を明らかにするために脳腫瘍患者末梢血中におけるT-cellの分布を測定し,さらに遅延型過敏反応であるツベルクリン反応(以下ツ反と略す)およびDinitrochlorobe—nzen塗布試験3,15,16)(以下DNCB試験と略す)との関連の上で脳腫瘍患者の細胞性免疫能を観察したので報告する。
A role of immune system in neoplastic disease has long been of great interest from etiological and therapeutic points of view. In the present studies patients with malignant neoplasm were found to have the depressed cell-mediated immunity.
We have already pointed out the depressed cell-mediated immunity in patients with brain tumor, particularly in those with glioma, which was indi-cated by 3H-thymidine uptake into blastic trans-formed lymphocytes to phytohemagglutinin (PHA). But it was unknown whether the fall of 3H- thymidine uptake was due to the decrease of T-cells in regularized lymphocytes or the dysfunction of several T-cell about DNA synthesis.
In order to clarify this problem, we measured the population of lymphocytes in peripheral venous blood and the subpopulation of the thymus-derivedlymphocytes (T-cell) in them. Lymphocytes were separated from heparinized venous blood by gravity segimentation method. T-cells were decided from the separated lymphocytes with sheep red blood cells which were the markers to form ROSETTE round the T-cell membrane.
Of all the patients with glioma, those with other brain tumor and control subjects, lymphocytes con-stituted 21±10%, 25±10% and 36±16% of their peripheral blood cells, 36±10%, 38±10% and 44± 12% of which were T-cells. Lymphocyte counts (T-cell counts) were 1167±545/mm3, 1947±1052/ mm3 and 2244±871/mm3 (486±309/mm3, 700+305/ mm3 and 915±208/mm3) in each group. T-cell percentages were similar to one another and there were no statistic differences between them. T-cell counts in patients with glioma were more decreased than those in the other two groups with statistic difference. It is certain that the decrease of T-cells in patients with glioma is due to the decrease of lymphocytes in their peripheral venous blood. And it is also certain that the fall of 3H-thymidine uptake in them will be affected not by the decrease of T-cells in regularized lymphocytes, but by thedysfunction of several lymphocyte.
On the other hand it is said that the suppressed blastogenic response of lymphocytes in correlated with the depression of the delayed hypersensitivity reactions (DHR), and accordingly the depression of them may also be affected by the dysfunction of several T-cell. In order to prove this supposition, it is necessary to clarify the existence of correlation between DHR and the counts of immuno-competent cell (lymphocyte and T-cell). We tested the DHR in patients with brain tumor with tuberculin and dinitrochlorobenzen (DNCB). Skin reactivity to tuberculin was depressed in them, particularly in those with glioma, but it was also depressed in a half of the control subjects. As to DNCB the skin reactivity was depressed in three-fourth patient with brain tumor and almost none of the control subjects was depressed. DNCB was, it was assumed, the better antigen to clarify the depressed cell-mediated immunity in patients with brain tumor than tuberculin. Whether patients have brain tumor or not, lymphocyte and T-cell counts tended to be decreased in cases with depressed DHR.
From the results as mentioned above, it is con-cluded that the depressed cell-mediated immunity in patients with brain tumor, including in those with glioma, is concerned with both the dysfunction of several T-cell and the decrease of T-cell counts in general. How to activate and how to increase the T-cells are the important problems to accomplish the treatment in patients with brain tumor.
Copyright © 1975, Igaku-Shoin Ltd. All rights reserved.


