Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.緒言
末端肥大症を伴う好酸性下垂体腺腫はしばしば糖尿病を合併する4)16)。われわれは最近術後急激に糖尿病が増悪した1例と術後急激に発症した1例を経験した。2例とも合併症,すなわち前者は真菌性髄膜炎により,後者は胃潰瘍穿孔性腹膜炎により死亡し,病理学的にその詳細を検討しえたので報告する。
Two cases of acromegaly with diabetes mellitus caused by eosinophilic pituitary adenoma were report-ed.
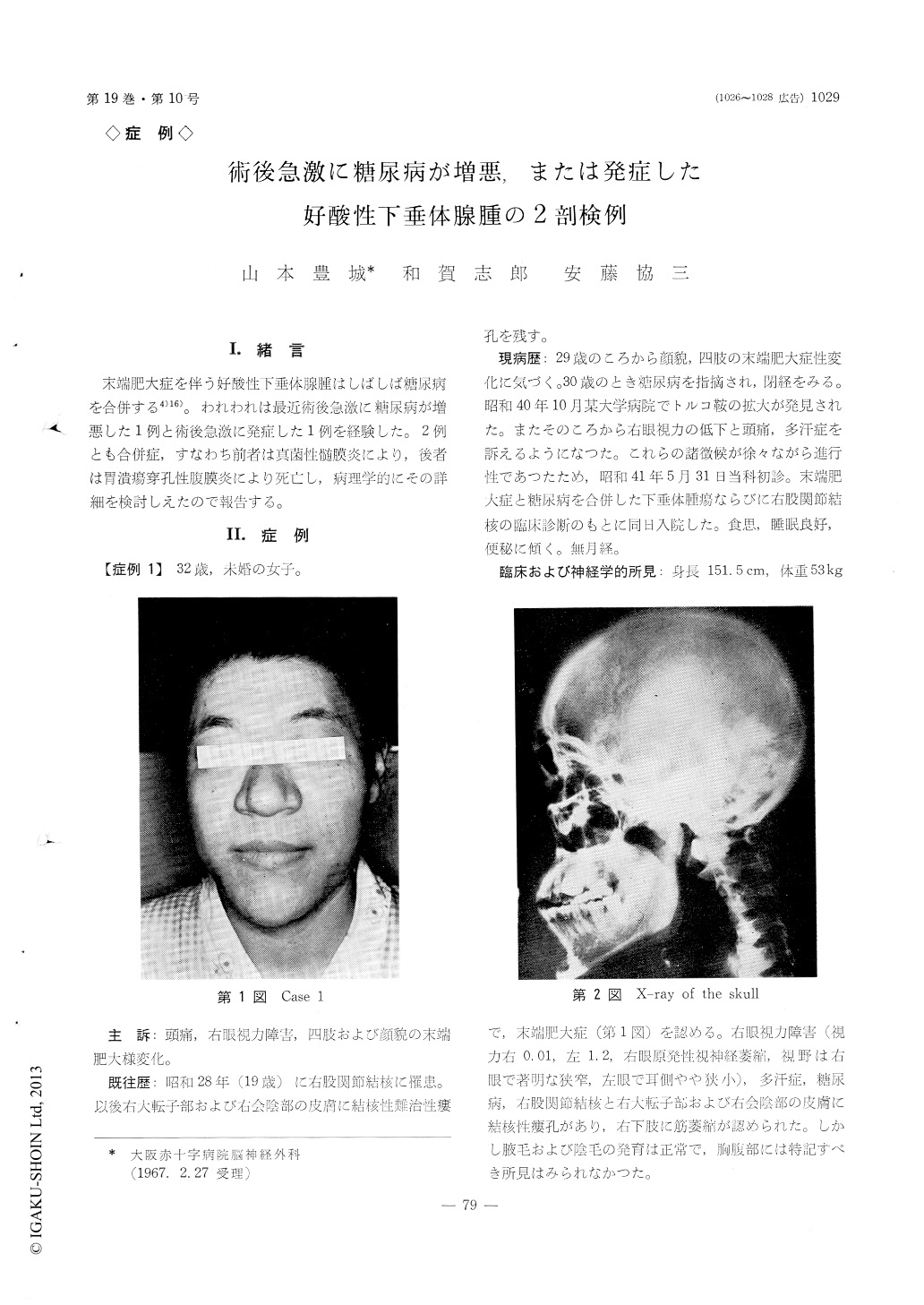
Case 1. A spinster, aged 32, was admitted to the Department of Neurosurgery of Osaka Red Cross Hospital on May 31, 1966. Her illiness began with acromegalic changes of facial features, hands and feet at 29 year-old in 1963, followed by glycosuria and cessation of menstruation.
At the time of admission, glycosuria and hypergl-ycemia were detected aside from a typical acromegalic overgrowth, hyperhidrosis, a ballooned sella, and pri-mary optic nerve atrophy and visual field defect of the right eye. The right tuberculous coxitis with fistulas in perineum and right thigh was also present.
A diagnosis of pituitary tumor with acromegaly and diabetes mellitus and right tuberculous coxitis was made clinically. Urinalysis showed 0.5% sugar andthe fasting blood sugar was 208 mg/dl.
Since the fasting blood sugar was controlled to the level of less than 140 mg/dl and urinary sugar to the level of less than 10g/day by the insulin and dietary treatment, the right transfrontal craniotomy was per-formed and the pituitary tumor was removed partial-ly. Histologically it was eosinophilic adenoma. A total dosage of 1955 mg of prednisolone was admin-istered during 26 days pre- and post-operatively for the purpose of substitution therapy as well as the treatment of cerebral edema.
She had uneventful postoperative course except for the moderate degree of hyperglycemia which devel-oped on the 4 th p. o. d. and was relatively insulin-resistant. On the 12 th p. o. d. she started to have low-grade meningitis, but bacteria could not be found in the CSF.
Although anti-biotics, hypertonic solution and con-tinuous ventricular drainage were applied, the patient was dead on the 20 th p. o. d.
Findings of the postmortem examination:
1) Basal meningitis with hemorrhage.
2) Ballooned and destroyed sells.
3) Remnant of pituitary tumor.
4) Acromegaly and visceromegaly.
Histological findings: 1) Distinct quantitative reduction with hyaline de-generation and fibrosis of islets of Langerhans.
2) Glycogenic vacuolization of liver cell nuclei.
3) Diabetic glomerulosclerosis of kidney.
4) Cell infiltration with fungi and giant cells in the leptomeninges of the interpeduncular cis-tern and in the ependyma of the 3 rd ven-tricle.
Case 2. A housewife, aged 42, was hospitalized on Jan. 9, 1966, with complaints of the coarseness of features and enlargement of extremities since 20 year-old visual disturbance of both eyes and amenorrhea since 23 year-old, and occasional abdominal pain since Dec., 1965.
On admission she was markedly acromegalic with clinical findings of the bilateral primary optic nerve atrophy, visual field defects and the ballooned sella. No sugar was found in urine and the fasting blood sugar was 108 mg/dl.
A clinical diagnosis of pituitary tumor with acro-megaly was made. She had an uneventful hospital course without dietary restrictions. On Jan. 24, 1966, an operation was performed on her by the usual left transfrontal route and the eosinophilic adenoma was partially removed. A total dosage of 845 mg of pre-dnisolone was given during 33 pre- and post-operative days as a substitution therapy.
She had rather quiet postoperative course until the 12 th p. o. d., when she started to have hyperglycemia, ranging from 346 mg/dl to 465 mg/dl, which could be controlled by the insulin treatment. However, she had the sudden onset of acute anemia and went into the secondary shock on the 17 th p. o. d. and died from clinically undetectable etiology on the 20 th p. o. d.
Autopsy findings:
1) Severe systemic anemia.
2) Localized peritonitis due to perforation of gastric ulcer.
3) Ballooned and destroyed sella.
4) Remnant of pituitary tumor.
5) Acromegaly and visceromegaly.
Histological findings:
1) Rather hypertrophic and proliferated islets of Langerhans without degeneration.
2) No diabetic change in liver and kidney.
Conclusion
1) Diabetes mellitus in the case 1 was thought to be pancreatic one originated from the pituitary and that in the case 2 to be pituitary origin.
2) Diabetogenic factors which caused a postop-erative aggravation of diabetes in the case 1 and the sudden onset of diabetes in the case 2 seemed to be mainly growth hormone and partially the steroid used.
3) Both cases died from respective complications, namely, monilial meningitis in the case 1 and acute localized peritonitis due to perforation of gastric ulcer in the case 2.
Copyright © 1967, Igaku-Shoin Ltd. All rights reserved.


