Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- 参考文献 Reference
- サイト内被引用 Cited by
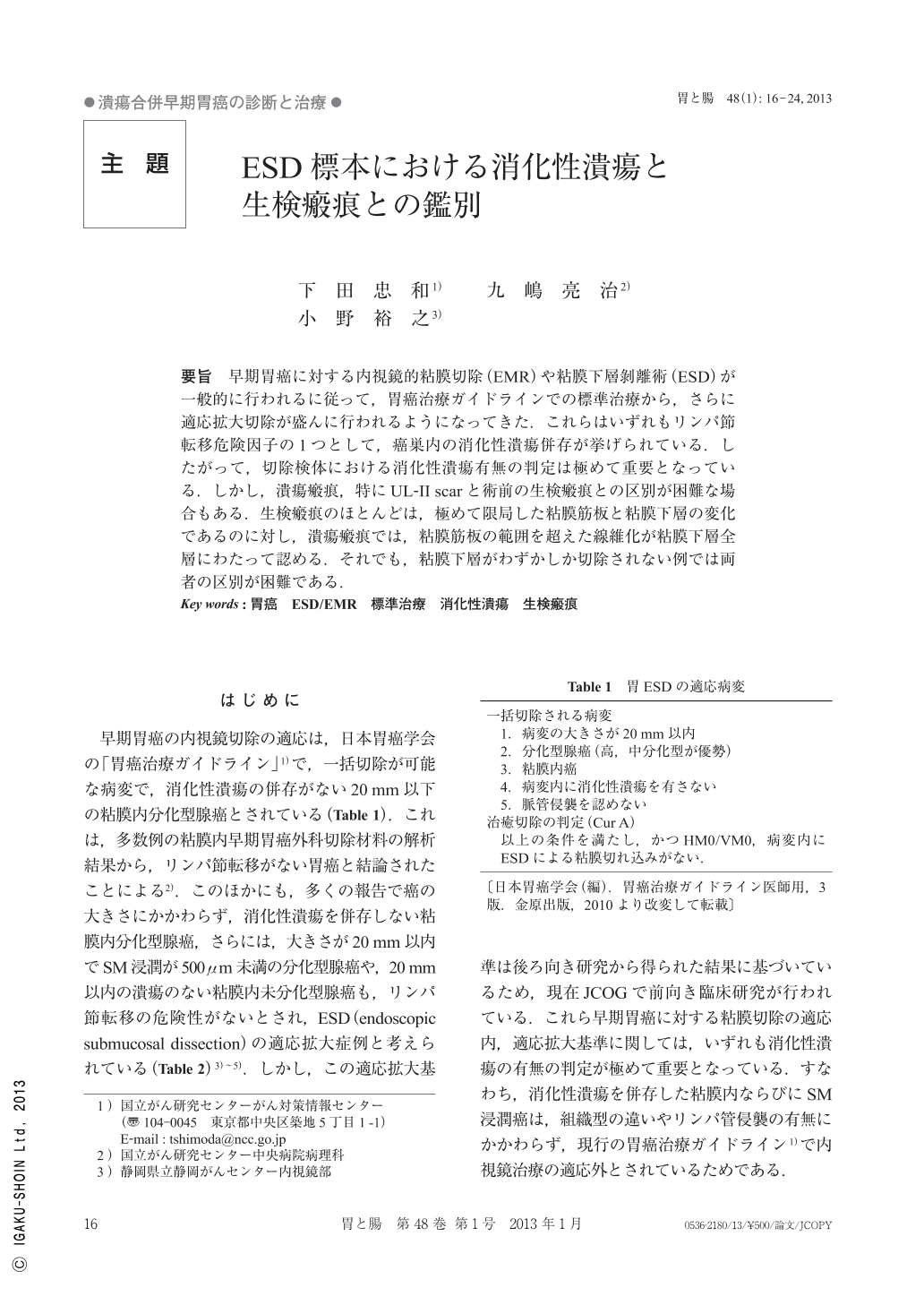
要旨 早期胃癌に対する内視鏡的粘膜切除(EMR)や粘膜下層剝離術(ESD)が一般的に行われるに従って,胃癌治療ガイドラインでの標準治療から,さらに適応拡大切除が盛んに行われるようになってきた.これらはいずれもリンパ節転移危険因子の1つとして,癌巣内の消化性潰瘍併存が挙げられている.したがって,切除検体における消化性潰瘍有無の判定は極めて重要となっている.しかし,潰瘍瘢痕,特にUL-II scarと術前の生検瘢痕との区別が困難な場合もある.生検瘢痕のほとんどは,極めて限局した粘膜筋板と粘膜下層の変化であるのに対し,潰瘍瘢痕では,粘膜筋板の範囲を超えた線維化が粘膜下層全層にわたって認める.それでも,粘膜下層がわずかしか切除されない例では両者の区別が困難である.
As EMR(endoscopic mucosal resection)and ESD(endoscopic submucosal dissection)for early gastric cancer are being more widely performed, resection with broader application than standard treatment according to the Gastric Cancer Treatment Guidelines is more frequently performed. The coexistence of peptic ulcer within carcinoma lesions is one of the risk factors of lymph node metastasis. Therefore, determining the presence of peptic ulcer in resected specimens is very important. However, it is sometimes difficult to differentiate between ulcer scars, especially UL-II scars, and scars from biopsy before surgery. Most biopsy scars are highly localized changes in the muscularis mucosae and submucosa, but ulcer scars display fibrosis of all submucosal layers, exceeding the range of muscularis mucosae.
However, the two are still difficult to differentiate when only a small amount of submucosa is resected.
Copyright © 2013, Igaku-Shoin Ltd. All rights reserved.


