Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
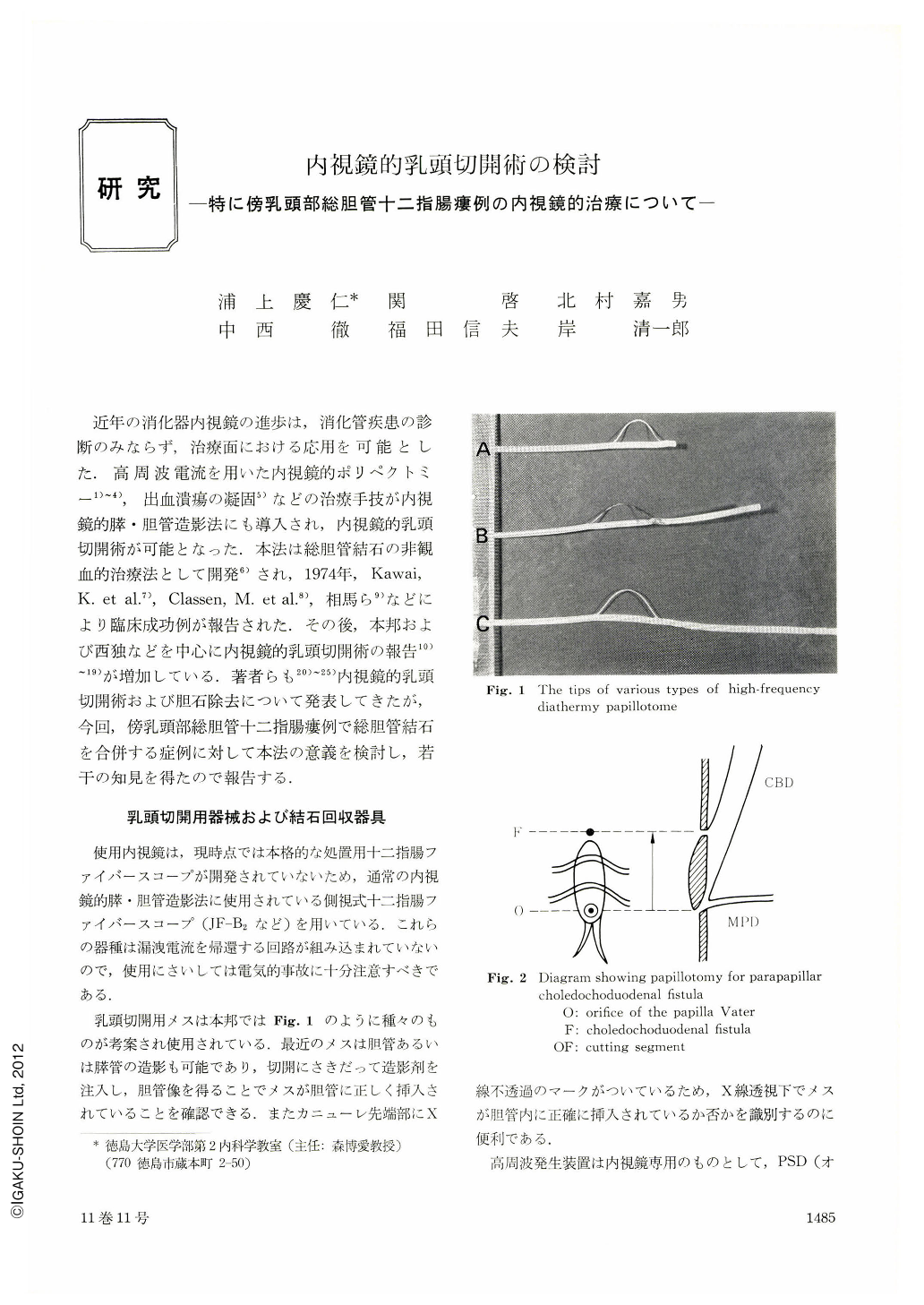
近年の消化器内視鏡の進歩は,消化管疾患の診断のみならず,治療面における応用を可能とした.高周波電流を用いた内視鏡的ポリペクトミー1)~4),出血潰瘍の凝固5)などの治療手技が内視鏡的膵・胆管造影法にも導入され,内視鏡的乳頭切開術が可能となった.本法は総胆管結石の非観血的治療法として開発6)され,1974年,Kawai,K. et al.7),Classen,M. et al.8),相馬ら9)などにより臨床成功例が報告された.その後,本邦および西独などを中心に内視鏡的乳頭切開術の報告10)~19)が増加している.著者らも20)~25)内視鏡的乳頭切開術および胆石除去について発表してきたが,今回,傍乳頭部総胆管十二指腸瘻例で総胆管結石を合併する症例に対して本法の意義を検討し,若干の知見を得たので報告する.
Endoscopic papillotomy for parapapillar choledochoduodenal fistula is reported and its significance is discussed.
The fistula is usually seen on the longitudinal ruga of the duodenal papilla or on its oral side. The scalpel for papillotomy is inserted into the common bile duct via the orifice of the duodenal papilla and then incision is made from the orifice through the fistula. With this technique the distal portion of the choledochus is largely opened. Therefore, this makes easy a spontaneous delivery of stones associated or removal of stones by an instrument. Since most cases of this fistula are associated with residual stones in the choledochus, this technique is a useful therapy for this disease.
On the other hand, in cases complicated reflux cholangitis regurgitated contents of the bile duct are more easily and immediately excreted into the duodenum after this procedure. That is, this technique is also useful for the treatment of reflux cholangitis associated with the fistula.
The stress of this technique imposed on the patients is very mild and it appears to be an indication of first choice even in those with postcholecystectomy or of poor risk.
Since the incision of the fistula from the orifice of the duodenal papilla is safely carried out without a danger of perforation, this is considered to be informative for the establishment of the length of incision in future endoscopic papillotomy.
Copyright © 1976, Igaku-Shoin Ltd. All rights reserved.


