Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
本邦における潰瘍性大腸炎は,難病対策研究班の発足以来,急速に活発となり注目されてきた疾患の1つである.
また,本症が慢性かつ難治性のため,合併症の併発の理由で手術される症例は,次第に増加している.その合併症の1つとして癌化の問題があり,欧米における頻度は1~4%であるが本邦報告例は,極めて稀である.
われわれは,12年前に潰瘍性大腸炎の診断にて結腸左半切除術を施行した残存直腸に,癌の発生した症例を経験したので,若干の文献的考察を加えて報告する.
症 例
患 者:49歳 主婦
主 訴:下痢 粘血便
家族歴:父が胃癌にて死亡
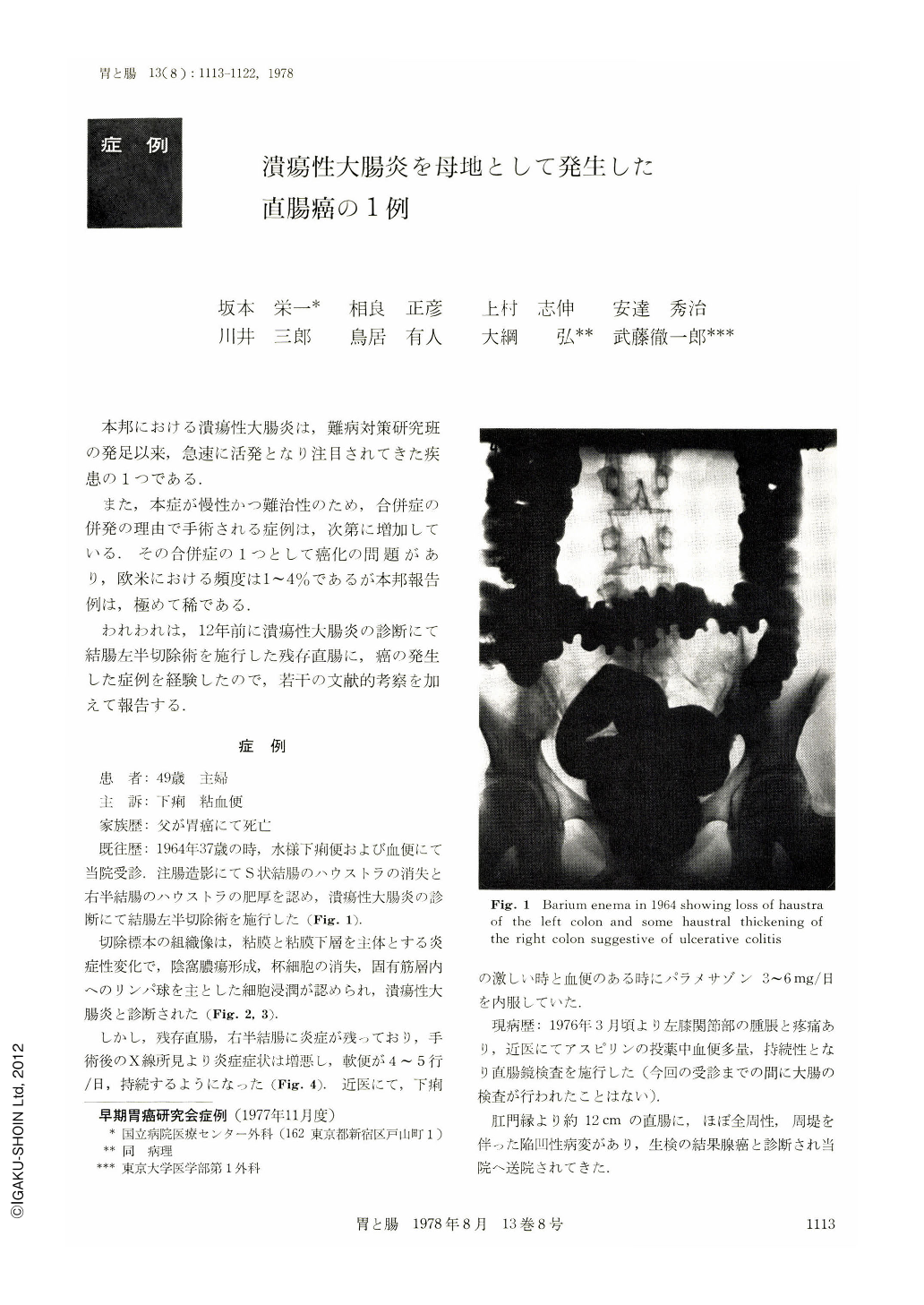
既往歴:1964年37歳の時,水様下痢便および血便にて当院受診.注腸造影にてS状結腸のハウストラの消失と右半結腸のハウストラの肥厚を認め,潰瘍性大腸炎の診断にて結腸左半切除術を施行した(Fig. 1).
切除標本の組織像は,粘膜と粘膜下層を主体とする炎症性変化で,陰窩膿瘍形成,杯細胞の消失,固有筋層内へのリンパ球を主とした細胞浸潤が認められ,潰瘍性大腸炎と診断された(Fig. 2,3).
しかし,残存直腸,右半結腸に炎症が残っており,手術後のX線所見より炎症症状は増悪し,軟便が4~5行/日,持続するようになった(Fig. 4),近医にて,下痢の激しい時と血便のある時にパラメサゾン3~6mg/日を内服していた.
現病歴:1976年3月頃より左膝関節部の腫脹と疼痛あり,近医にてアスピリンの投薬中血便多量,持続性となり直腸鏡検査を施行した(今回の受診までの間に大腸の検査が行われたことはない).
肛門縁より約12cmの直腸に,ほぼ全周性,周堤を伴った陥凹性病変があり,生検の結果腺癌と診断され当院へ送院されてきた.
A 49-year-old woman visited our hospital with a complaint of severe continuous bloody stools for the past two years. She had undergone left hemicolectomy with transverso-sigmoidostomy for ulcerative colitis 12 years previously, and since then she had been occasionaly treated by oral steroid when she had episodes of diarrhea or bloody stool.
On admission routine blood test revealed anemia, hypoalbuminemia and marked elevation of serum CEA. Barium enema showed loss of haustra, multiple erosions of the residual colon and stenosis of the rectosigmoid. On colonoscopy the mucosa was reddish and edematous with multiple erosions, but no evidence of carcinoma was detected. Multiple biopsies of the stenotic site revealed poorly differentiated adenocarcinoma with dysplastic or precancerous change of the surrounding mucosa. Proctocolectomy with modified Kock's‘continent ileostomy’was performed. Postoperative course was uneventful.
Operative specimen showed dark-reddish mucosa with fine granularity of the whole colon. Apart from marked thickening of the bowel wall at the site of stenosis no definite findings suggestive of malignancy were noticed. The whole specimen was examined microscopically by step serial sections of 5 mm width in an attempt to find distribution of cancer and precancerous change of the mucosa. The main tumor was advanced carcinoma of mixed, well and poorly differentiated adenocarcinoma with lymph node metastasis. It was surrounded by wide area of carcinoma with submucosal invasion and carcinoma in-situ. There were multiple foci of carcinoma in-situ and a focus of invasive carcinoma only distal to the main tumor. All the remaining mucosa was convered by irregular tubules with variable degree of dysplasia, suggestive of precancerous change. There were multiple well differentiated, poorly differentiated and signet-ring cell carcinomas present in the surrounding mucosa. There was no active inflammation or normal mucosa in the specimen. This is a typical example of multiple colon cancer complicating ulcerative colitis with a 12-year history and probably the first histologically well described case in this category in Japan.
Copyright © 1978, Igaku-Shoin Ltd. All rights reserved.


