Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- 参考文献 Reference
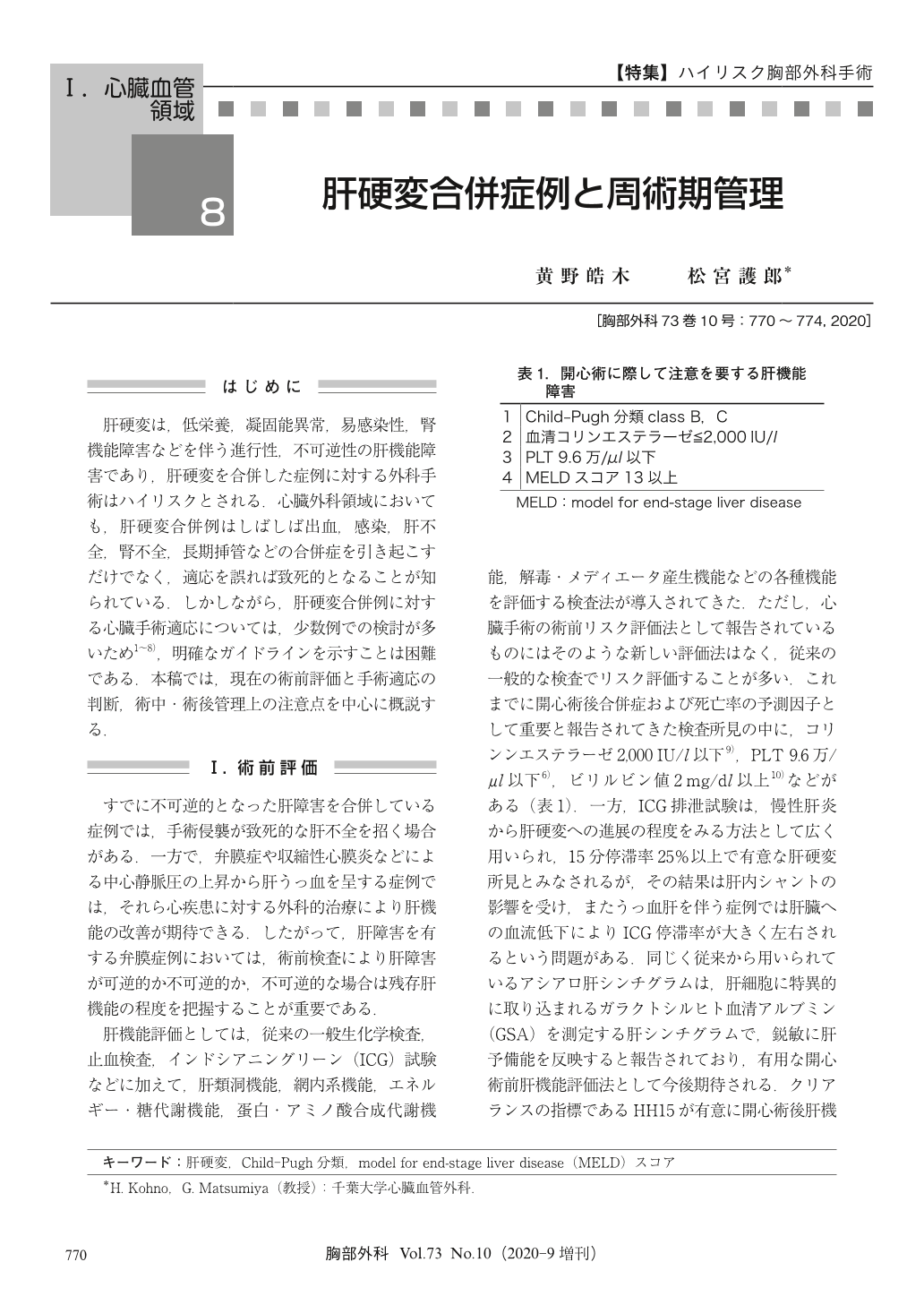
肝硬変は,低栄養,凝固能異常,易感染性,腎機能障害などを伴う進行性,不可逆性の肝機能障害であり,肝硬変を合併した症例に対する外科手術はハイリスクとされる.心臓外科領域においても,肝硬変合併例はしばしば出血,感染,肝不全,腎不全,長期挿管などの合併症を引き起こすだけでなく,適応を誤れば致死的となることが知られている.しかしながら,肝硬変合併例に対する心臓手術適応については,少数例での検討が多いため1~8),明確なガイドラインを示すことは困難である.本稿では,現在の術前評価と手術適応の判断,術中・術後管理上の注意点を中心に概説する.
Liver cirrhosis is a major risk factor in patients requiring cardiac surgery. Although current evidence is limited to reports coming mostly from small case series, it is clear that the surgical risk increases with the severity of the liver disease. Hemodynamic instability caused by hyperdynamic circulation, systemic fluid retention, infection, and bleeding is frequently observed postoperatively in severely cirrhotic patients. Preoperative optimization, including correction of coagulopathy and poor nutrition, is therefore crucial for minimizing the predictive postoperative complications in those patients. Postoperative management should focus on bleeding and infection control, body fluid management, adequate nutrition, and hemodynamics, particularly hepatic circulation. Multiple studies have shown that patients who are diagnosed as Child-Pugh class B or C liver cirrhosis have a high surgical mortality rate, with most reports suggesting class C as inoperable. Recently, the model for end-stage liver disease (MELD) score has been gaining attention for its reliability in identifying patients at high risk for open heart surgery. Off-pump surgery may be beneficial in improving the surgical outcomes, but the evidence is weak and further studies are required. A thorough preoperative evaluation is thus mandatory in cirrhotic patients scheduled for cardiac surgery, with a particular attention to the risks and benefits of performing the surgery itself.
© Nankodo Co., Ltd., 2020


