Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
1.緒言
頭部外傷後に起る痙攣発作は通常大きく二つに分けられる。すなわち,受傷後早期に出現するものを早期てんかん(early epilepsy),一定期間たつてから起るものを晩期てんかん(late epilepsy)という。早期てんかんと晩期てんかんを区別する時期については意見の分れるところであるが,受傷後1週間以内のものを早期てんかんそれ以後のものを晩期てんかんとする Jennett3〜5)の分け方が多く採用されている。さらに,受傷後24時間以内に発症する痙攣を直後てんかん(immediate epilepsy)として早期てんかんと区別する意見もあるが(Walker23)大田原13),Kollevold6〜8)),この両者の異同は明らかでなく,ほとんどの場合早期てんかんに含めて取扱われている。外傷後の頭蓋内の状況は日時を追つて当然変化すると考えられるから,直後てんかんとその後の早期てんかんの発生機序が異なつても不思議ではないが,臨床上の諸問題とのかかわりにおいて,この両者の占める重要性に差はない。発生頻度からは直後てんかんの方がはるかに高く(早期てんかんの70〜80%前後5,15)),われわれの施設における頭部外傷例においても,早期てんかんの77%は直後てんかんであつた。
Posttraumatic epilepsy is usually devided into three categories, namely, immediate, early and late epilepsy.
The immediate epilepsy or convulsion is defined as the seizure occuring within the first twenty-four hours after head injury.
This type of convulsion is encountered in emer-gency medical practice frequently and also con-sidered as one of the most important problems in head injury management. The incidence of post-traumatic immediate convulsion in our University Clinic is 5.7% (101 cases of 1.757 head injuries), very similar to those in other clinical reports.
Immediate posttraumatic convulsion itself has been thought to have good prognosis. But, it often accompanies depressed fracture, cerebral contusion and intracranial hematoma, and in these cases pa-tients fall down into more severe condition.
A few authors reported that the incidence of late traumatic epilepsy was higher in those patients who had early posttraumatic epilepsy-most of them was immediate posttraumatic convulsion, than in those who did not.
It is much important for us to investigate the pathophysiological processes of immediate post-traumatic convulsion and to offer it's prophylactic and therapeutic methods in clinical practice.
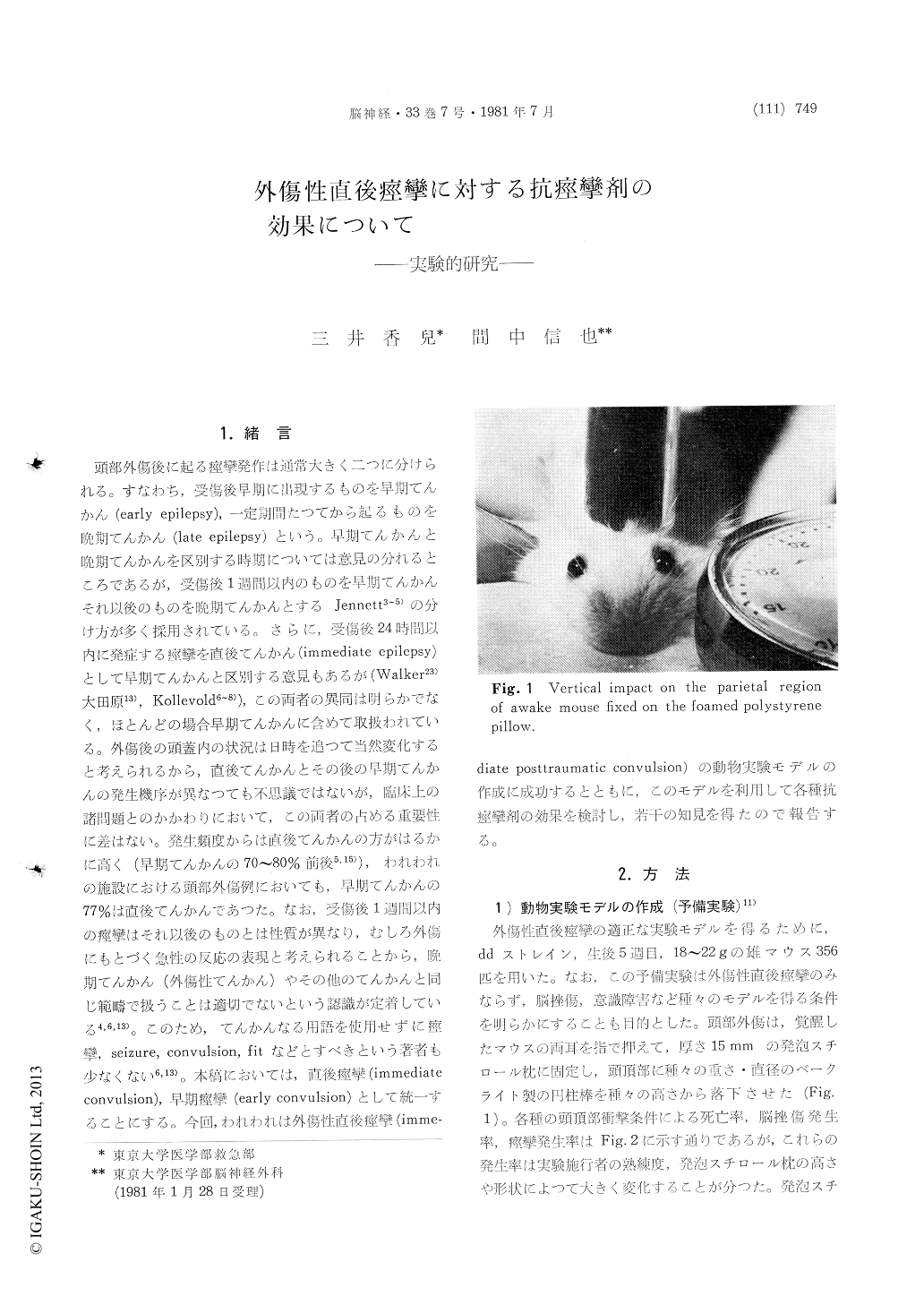
We have been able to get the adequate experi-mental model of immediate posttraumatic convul-sion with dd strain mice when we give the vertical impacts to the parietal region of the awake mice (18-22g) fixed by fingers on foamed polystyrene pillow, with bakelite cyllinder stick of 30g in weight, 10 mm in diameter, from the hight of 30 cm, through the plastic tube. With this experi-mental model we examined the effectiveness of various anticonvulsants to immediate posttraumatic convulsion.
30 minute prior to impact, each anticonvulsant, phenobarbital (PB), phenytoin (diphenylhydantoin, DPH), diazepam (DZP), carba mazepine (CBZ), valproic acid (VPA), was administered intra-abdo-minally.
Soon after the convulsion or 10 minutes later when the convulsion was not occured, the blood samples were taken for the determination of the serum concentration of anticonvulsants.
PB and DPH were measured by UV (Ultra Violet) spectrophotometry developed by Saito which is adopted in our clinic for routine monitoring of PB & DPH, required only 0.2-0.4ml of serum.
DZP, CBZ and VPA were measured by gaschro-matography. After the experiment, postmortem examination were performed, and the mice with cerebral contusion and/or intracranial hematoma were excluded. Each anticonvulsant showed linear corelation between administrated dose and serumconcentration. About the effectiveness of each anticonvulsant for immediate posttraumatic con-vulsion, PB, DZP, CBZ and VPA could suppress or control the seizure, but DPH showed no effec-tive action. Effective serum level of PB, DZP, CBZ and VPA, was above 15μg/ml, 0.983μg/ml, 2.76μg/ml and 352μg/ml, each of which, except VPA, lies within or near the limitation of our clinical use.
The effectiveness of these anticonvulsants for immediate posttraumatic convulsion suggests that the pathophysiological process of immediate post-traumatic convulsion is different from other epi-leptic convulsions including late posttraumatic epilepsy. And in our clinical practice, it could be mentioned that PB, DZP and CBZ may be available for the prophylaxis and the treatment of immediate posttraumatic convulsion.
Considerring that the most of these convulsions occur within one hour after the head injuries, it is necessary for serum anticonvulsant level to reach effective level as soon as possible. For this purpose intravenous administration of DZP and subsequent administration of PB (long half life) may be rec-ommended.
Copyright © 1981, Igaku-Shoin Ltd. All rights reserved.


