Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
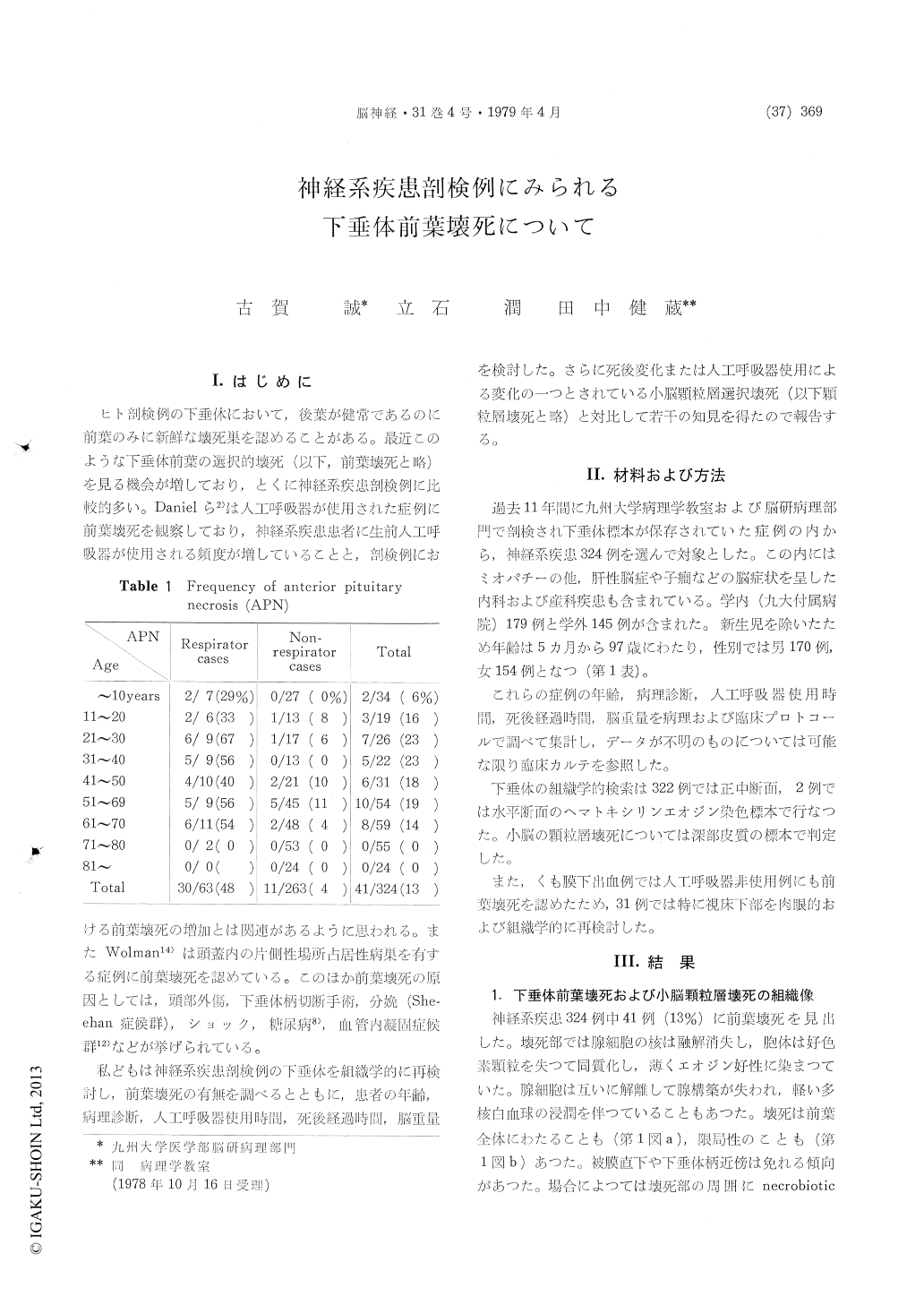
ヒト剖検例の下垂体において,後葉が健常であるのに前葉のみに新鮮な壊死巣を認めることがある。最近このような下垂体前葉の選択的壊死(以下,前葉壊死と略)を見る機会が増しており,とくに神経系疾患剖検例に比較的多い。Danielら2)は人工呼吸器が使用された症例に前葉壊死を観察しており,神経系疾患患者に生前人工呼吸器が使用される頻度が増していることと,剖検例における前葉壊死の増加とは関連があるように思われる。またWolman14)は頭蓋内の片側性場所占居性病巣を有する症例に前葉壊死を認めている。このほか前葉壊死の原因としては,頭部外傷,下垂体柄切断手術,分娩(She—ehan症候群),ショック,糖尿病8),血管内凝固症候群12)などが挙げられている。
私どもは神経系疾患剖検例の下垂体を組織学的に再検討し,前葉壊死の有無を調べるとともに,患者の年齢,病理診断,人工呼吸器使用時間,死後経過時間,脳重量を検討した。さらに死後変化または人工呼吸器使用による変化の一つとされている小脳顆粒層選択壊死(以下顆粒層壊死と略)と対比して若干の知見を得たので報告する。
In order to evaluate the incidence of anterior pituitary necrosis (APN) at autopsy and to investi-gate its pathogenesis, the survey of 324 autopsy cases with various neurological disorders was per-formed. Available clinical data, macroscopic findings, and histological slides were examined.
Histopathological diagnosis of fresh APN was made in 41 cases (13%) without appreciable alterations in the posterior pituitary. Their age ranged from 6 to 70 years, and APN was relatively rare in children and aged persons.
A respirator had been used prior to death in 30 cases among them. APN was present in 23 (62%) out of 37 cases whose respiration had been con-trolled by means of a respirator for longer than a day. In most of them APN was extensive, sometimes associated with a thin rim of surviving glandular cells at the periphery and in the area adjacent to the pituitary stalk. On the other hand,the patients who had undergone long-term but only assistant respirator therapy, for example the patients of myasthenia gravis, did not necesssrily show APN. We considered that selective necrosis of the anterior pituitary in respirator cases was probably due to the difference of metabolic activities between the anterior and posterior pituitary.
APN was also recognized in 11 non-respirator cases, including the patients of subarachnoid hemorrhage due to intracranial aneurysm (6), head trauma (1), cerebral hemorrhage (1), tuberculous meningitis (1), periarteritis nodosa (1), and encephalopathy due to postpartum hepatitis (1).
There was no positive correlation between the presence of APN and the time interval between death and autopsy. A certain extent of correlation was pointed out between the status bullosus (acute selective necrosis in the granular layer of the cerebellar cortex) and that of APN (correlation coefficient, +0.55). In spite of the absence of status bullosus, APN was observed in 12 cases including 3 of subarachnoid hemorrhage.
Excepting the children 10 years of age or younger, the mean brain weight of 39 cases with APN was by 130 g greater than that of 252 caseswithout APN. On the other hand, the mean brain weight of 56 respirator cases was also greater than that of 290 non-respirator cases irrelevantly to the presence or absence of APN. So we failed to confirm that increased brain weight itself caused APN.
Among 25 non-respirator cases of subarachnoid hemorrhage due to intracranial aneurysm, 6 showed focal APN. Their ruptured aneurysms were located on the anterior communicating artery in 4, and on the internal carotid in 2.
Two of these 6 cases grossly and histopatho-logically lacked necrosis and hemorrhage in the thalamus. It was our speculation that APN in the non-respirator cases of subarachnoid hemor-rhage was attributed to vasospasm of the artery supplying the pituitary, resembling cerebrovascular vasospasm. The latent hypofunction of the anterior pituitary, which was sometimes evident after the attacks of subarachnoid hemorrhage, might be partly due to APN.
It was noteworthy that APN was often noticed in the autopsy cases with various neurological disorders.
Copyright © 1979, Igaku-Shoin Ltd. All rights reserved.


