Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
1977年,Grüntzig1)らによって始められたPTCA(percutaneous transluminal coronary angioplasty)は,狭心症2〜5)および心筋梗塞6〜8)に対してその有効性が高く評価されている反面,多くの合併症を生ずる危険性がある。
side branch injury (SBI)(side branchの閉塞および狭窄)は,PTCAの合併症の1つであるが,その予後は比較的良好と考えられている。しかし,大きなside bra—nchの場合は心筋梗塞や狭心症を発生させる危険性があり充分な注意が必要である。
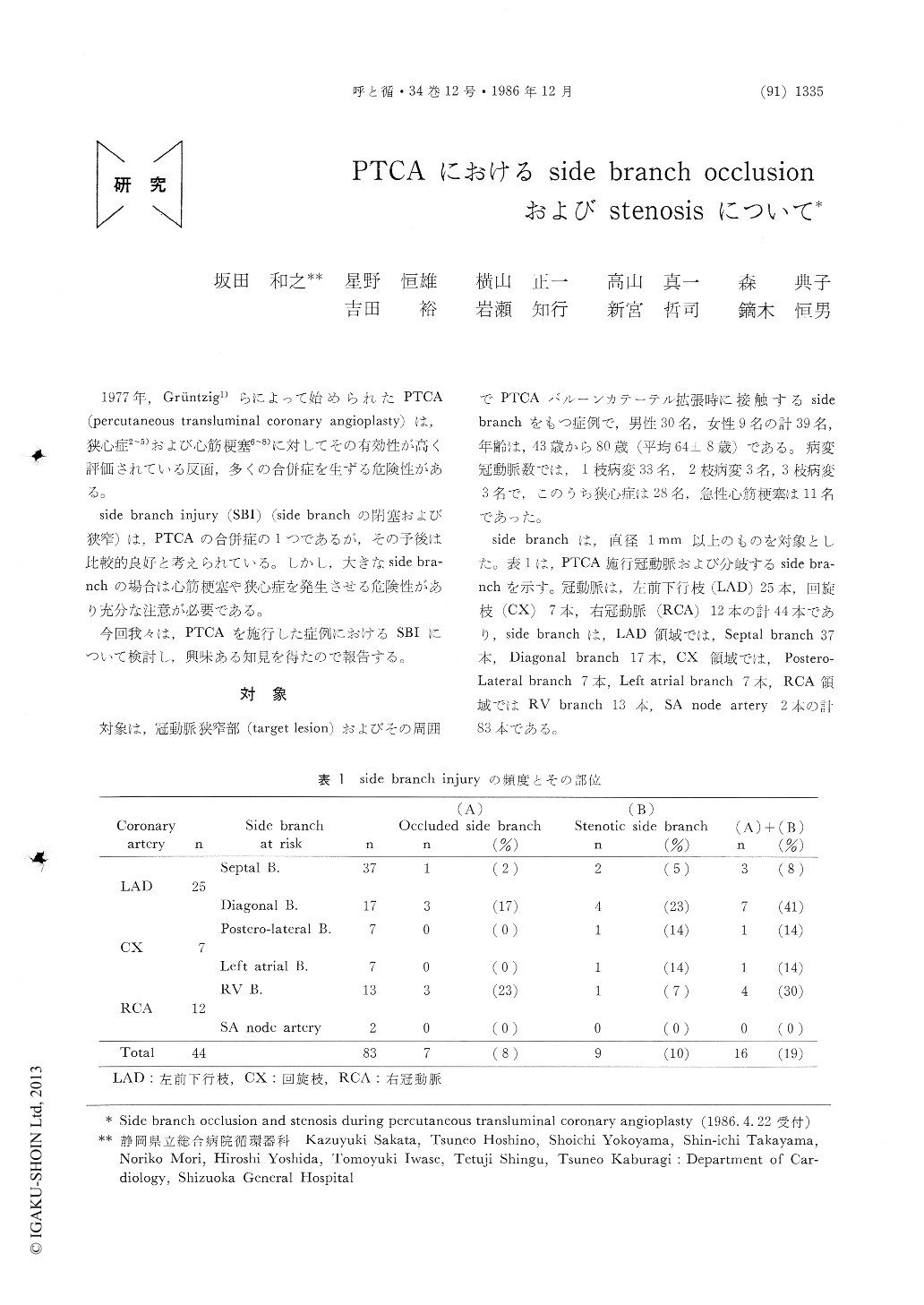
To assess the incidence and significance of side branch injury (SBI) including side branch occlusion and stenosis during percutaneous transluminal coronary angioplasty (PTCA), 44 coronary arteries with 83 side branches were analyzed from 39 patients treated by PTCA. We investigated the relationship between SBI and several factors; branching portion of the side branch, balloon diameter and pressure, and anatomical characteristics of the target lesion.
SBI occurred in 16 (19%) of 83 side brancheo following PTCA (7 occlusion, 9 stenosis). SBI occurred in 14 of 35 side branches originating from the target lesion and in 2 of 48 side branches originating from the vicinity of it. The incidence of SBI was significantly higher in the former than in the latter (p<0.01). The target lesion with SBI tended to be diffuse and eccentric and to have tortuosity and calcification. In addition, the target lesion with SBI was considered to be tight because luminal enlargement of target lesion with SBI was smaller than that without SBI (p< 0. 01). There was no significant relationship bet-ween SBI and balloon diameter and pressure. No patients with side branch stenosis had an elevation of CPK and ECG changes after PTCA. Two of 4 patients with angina pectoris, who had side branch occlusion, had myocardial infarction after PTCA. We must be cautious of the target lesion with side branch during PTCA.
Copyright © 1986, Igaku-Shoin Ltd. All rights reserved.


