Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- サイト内被引用 Cited by
術前における胃癌浸潤範囲の診断は,胃切除線の決定,手術方法の選択などに際して不可欠であり,その診断の精度は臨床に直結する重要な問題である.癌・非癌といった質的診断は病巣内のもっとも著しい所見を基礎にしてなされるため,X線,内視鏡検査とも特殊な例を除いて比較的容易になされるようになった.しかし,癌巣辺縁部は辺縁隆起を伴うような型を除いて陥凹型癌では,原則として周辺に至るほど表面所見は軽微になる傾向にあり,その浸潤辺縁部の診断には,Ⅱb型早期胃癌の診断概念を導入しなければならない例が少なくなく1),現状では多くの困難を伴う.
われわれは2),Ⅱb症例の検討からX線的,内視鏡的に本病変を診断するためのもっとも手近な方法の1つは胃小区像を描出することであり,その異常から本病変の存在と範囲を推定できるであろうと考え,X線および内視鏡検査において胃小区描出のために種々の努力を重ねてきた.内視鏡ではすでにいくどか報告3)~8)しているように,色素液を用いた「コントラスト法」(従来の色素撒布法に相当する,第19回内視鏡学会総会に併催された色素内視鏡研究会において改名された)により,また最近では胃X線検査に粘液溶解法を応用する9)~11)ことにより,両検査ともほぼ満足すべきところまで胃小区の描出が可能になった.色素内視鏡による癌の浸潤範囲と深達度診断に関してはすでに報告しているが12)~15),今回はとくに陥凹型胃癌の浸潤境界の診断を主として色素内視鏡(コントラスト法,染色法)の立場からとりあげ,通常内視鏡検査との対比の上からその有用性について述べてみたい.
The diagnosis of cancer borders was studied histologically and endoscopically.
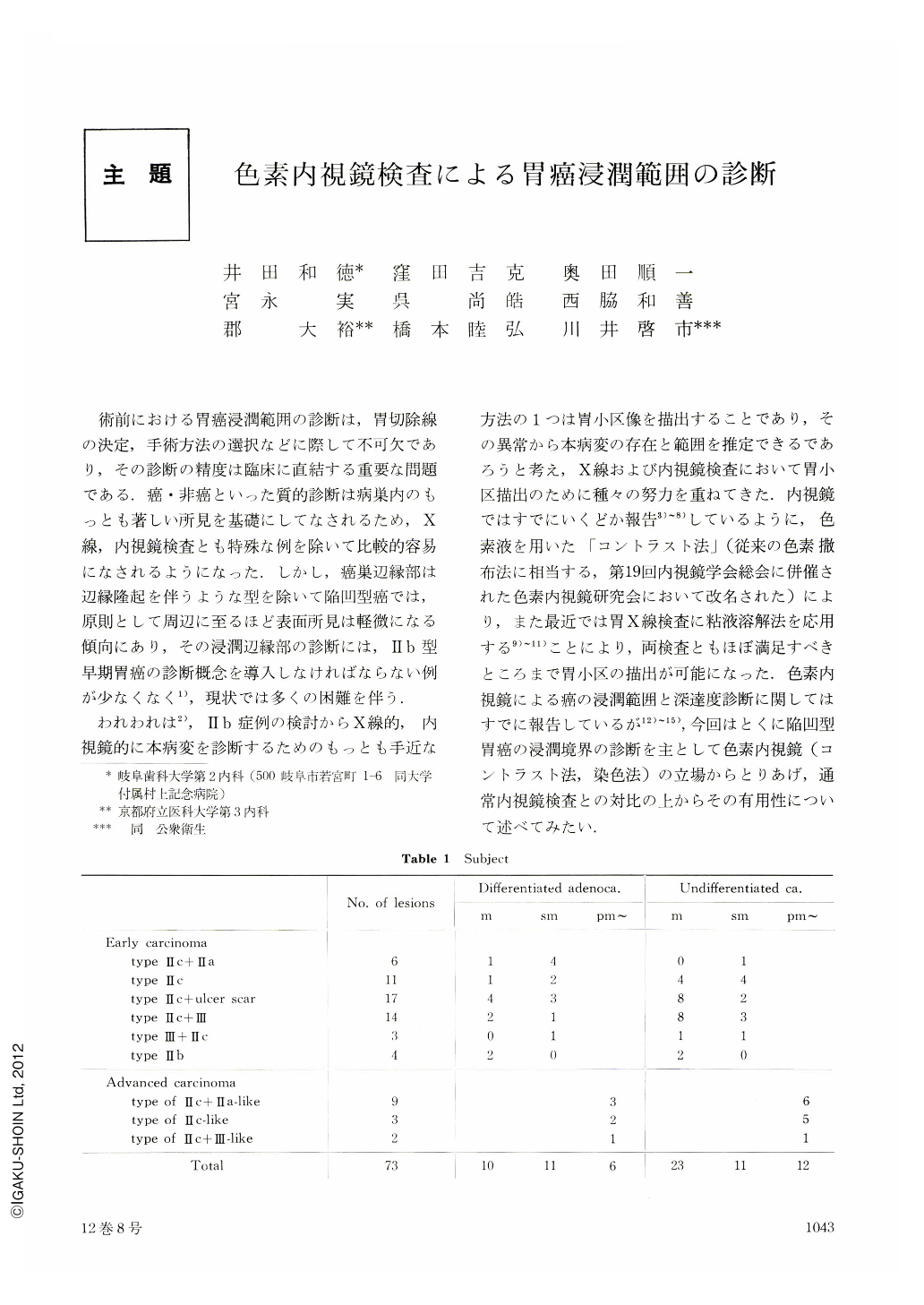
Contrast method including indigocarmine method, congo red-evans blue method and methylene blue staining method was performed on 69 lesions of depressed cancer and 4 lesions of type IIb early cancer of the stomach.
1) Differentiated adenocarcinoma of the stomach differed from undifferentiated carcinoma in the marginal infiltration. In the former, cancer nests exposed in 92% of the lesion at the marginal area. The depression, where cancer exposed, was generally shallow and unclearly demarcated. The latter lesions generally had marked depression, althogh the depressed margins with exposed cancer nest were seen in only 63%. The middle layer infiltrating type, which invaded into intermediate layer of the gastric mucosa beyond the depression, was seen in 36% of lesion composed of undifferentiated carcinoma.
2) Both histological types of gastric carcinoma can be differentiated with dye endoscopy on the basis of the relation between fundic-pyloric glandular border and site of lesion, with reference to the grade of intestinal metaplasia in the surrounding mucosa.
3) Diagnosis of the cancer border was more difficult by routine endoscopy than by macroscopic examination of the resected specimen, because routine endoscopy was inferior in delineating minimal depression in the gastric mucosa.
4) The cancer border was diagnosed more easily by contrast method than by macroscopic examination of the resected specimen, because contrast method clarified marginal depression of the lesion and visualized abnormal areae gastricae. With contrast method, the cancer border could be almost outlined in 73% of the lesion composed of undifferentiated carcinoma, and in 91% of the lesion composed of differentiated adenocarcinoma, while with routine endoscopy in less than 50% out of both histological types of the gastric cancer.
5) The cancerous lesions of middle layer type were hardly diagnosed with routine or dye endoscopy. The lesions showed minimal mucosal findings such as discoloration, depression, elevation and abnormal areae gastricae in the marginal area of undifferentiated carcinoma. The extent of this type was occasionally suggested with methylene blue staining.
6) Endoscopy employing the contrast method was generally effective in diagnosis of type IIb early gastric cancer composed of differentiated adenocarcinoma. Combination of the contrast and staining method was effective in diagnosis of extensive lesion of type Ⅱb cancer with middle layer type.
7) Contrast method should be applied to diagnosis of extent of cancerous infiltration for detailed examination. Methylene blue staining method should be applied in aids of diagnosis on the suspicion of type Ⅱb lesion or middle layer infiltration.
Copyright © 1977, Igaku-Shoin Ltd. All rights reserved.


