Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
アルコール多飲が慢性膵炎の病因として占める比率の高いことは各国の統計によって明らかである1)2).アルコール多飲者の飲酒量,酒の種類,飲酒期間と慢性膵炎の関係は,大量かつ長期間の飲酒者に本症が多いこと以外には一定の傾向がない.慢性膵炎を臨床的に診断するにはいろいろな方法があるが,大井3),高木4)によって実用化された内視鏡的膵管造影法はもっとも有効な手段の1つで,膵炎の診断には血管造影法より優れた結果がでている5).
スウェーデンでは内視鏡的膵管造影法は1971年マルメのL. Wehlinによってはじめて行なわれ,その後急速に発展し,現在北欧3国で盛んに施行されている.スウェーデンにはアルコール中毒者が多く,これは昔からのつよい飲酒習慣と陰うつな天候が主な原因で,その他の要因として完備した社会保障制度によりアルコール中毒になっても生活の心配がないこと,労働時間が短いこと,社会主義によるすべての平等化が行なわれ,労働量の多少にかかわらず賃金がほぼ同じであるので労働意欲の低下があること,および,政府のアルール販売制限策が逆効果になっていることなどが考えられる.
Alcohol is an important factor in the causation of pancreatitis (Table 7). From October 1972 to December 1973, endoscopic pancreatography and determination of serum amylase isoenzyme were carried out on patients with chronic alcoholism in Malmo General Hospital in Sweden. The purpose of this examination is to evaluate alcoholic pancreatitis.
Material
Medical and social signs of alcoholic disease.
This material consists of patients with known chronic alcoholism and fulfills the three cardinal criteria of alcoholic disease, namely :
1) “Black-outs” defined as a temporary loss of memory in conjunction with the consumption of alcohol which, according to Jellink, is an early symptom of alcoholic disease.
2) Uncontrolled drinking is according to Goodwin et al. related to chronic alcoholism and may be the best criterion.
3) “Restorer” defined as a physical dependence on alcohol after withdrawal following a drinking bout.
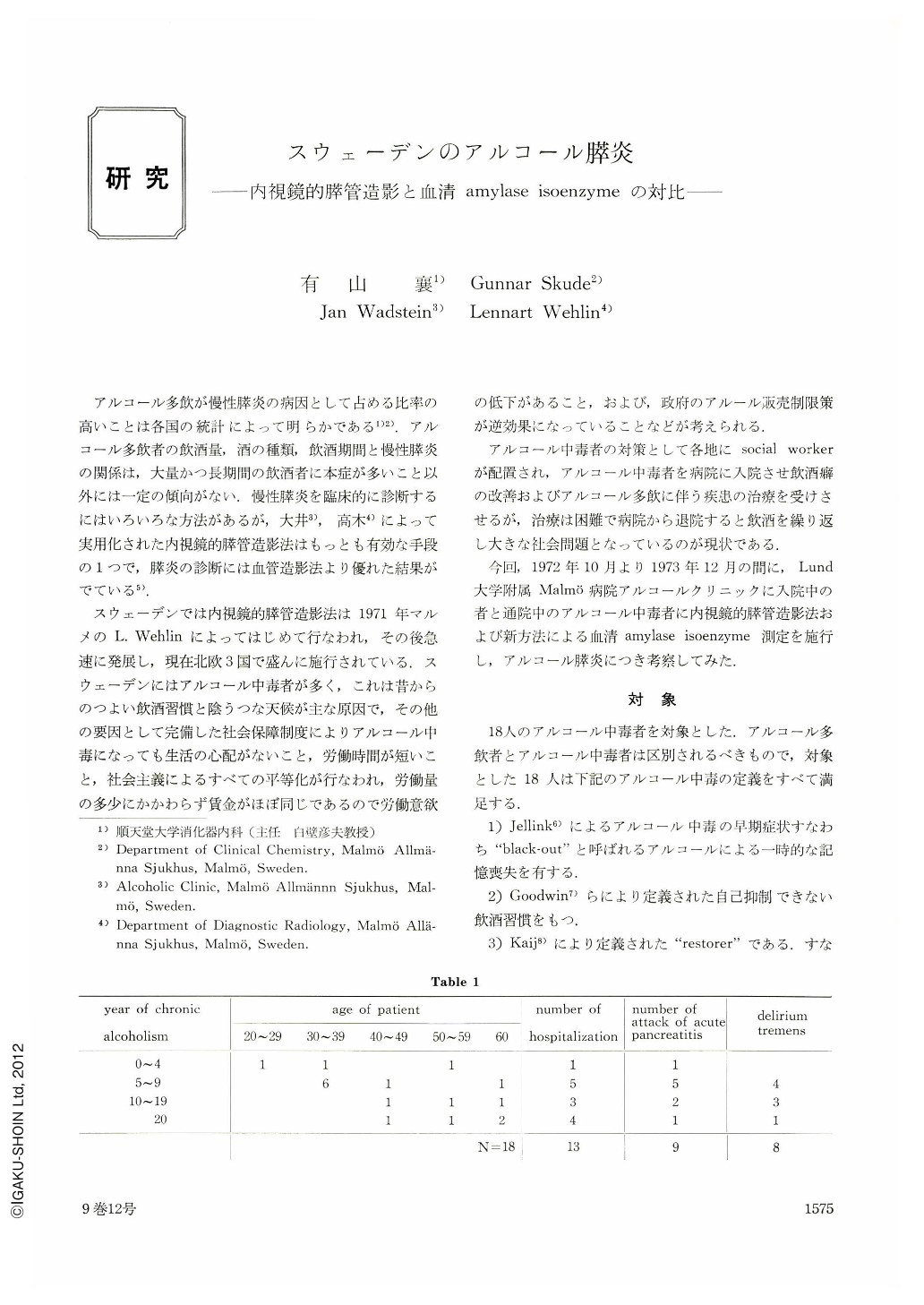
All patients except one have been treated at the alcoholic clinic of Malmo General Hospital. A good social sign of alcoholism is the number of entries in the Board of Excise register, where all but three patients are registered. The heavy drinking time which precedes the chronic alcoholism is difficult to judge because only the real time of chronic alcoholism is noted as seen from Table 1. From Table 1, we can see that nine patients have had pancreatitis one or more, and eight patients have had one or more delirium tremens.
Determination of serum amylase isoenzyme.
Laboratory thechniques.
Sesum amylase activity was determined with Phadebas Amylase Test (Pharmacia, Uppsala, Sweden) essentially in accordance with the manufacturer's instruction. For determination of the isoenzyme pattern of serum amylase agarose gel electrophoresis was performed according to Skude (1973) with the equipment described by Johansson (1972).
A 0.1 M barbitalsodium barbital buffer, pH 8.8, containing 1 mM calcium lactate was used in the buffer reservoirs as well as in the gel. The concentration of agarose (purchased from Miles-Selavic, Maidenhead, England, batch 269 A) in the gel was 0.8 per cent to reduce the electroendosmotic flow through the gel, it also contained 0.6 per cent linear polyacrylamide polymers. The thickness of the gel was 1.1 mm, which was filled with 9 μl sample. The electrophoretic separation time was two hours at 230 V (about 18 V/cm) ; the temperature of the cooling water was 10℃. After electrophoresis, the agarose gel on the anodal side of the slits was covered with a mixture of Phadebas Amylase Test tablets in 0.1 M phosphate buffer, pH 7.0 (7 tablets/ 10 ml.). This buffer also contained 0.5 per cent human serum albumin, 0.9 per cent sodium chloride and 1 per cent potassium chloride. After incubation in a moist chamber at 56℃ for 2.5 hours, the reaction mixture was washed off and the glass plate with the gel was fixed in methanol : acetic acid : distilled water (5 : 1 : 5). Then the gel was covered with a filter paper and dried in a current of warm air.
With this technique it is possible to identify three salivary amylase fractions and three pancreatic amylase fractions in cases with high serum amylase activities. At very low serum amylase levels, it is just possible to identify the main fractions of salivary and pancreatic amylase respectively. With some experience, the relative strength of the normally occurring salivary and pancreatic amylase isoenzyme was easily recognized and the use of a scanning procedure instead of direct inspection of the electrophoretic pattern for evaluating the isoenzyme pattern was unnecessary.
Figure 1 shows amylase isoenzyme pattern after electrophoretic separation of serum, anode above. “S” denotes main salivary separation ; “P” denotes main pancreatic fraction. The upper row of figures states total serum amylase activity, and the lower row the activity of the pancreatic fraction. Sample 1 and 2 represent normal isoenzyme pattern ; it shows roughly the same amount of salivary and pancreatic amylase. Sample 3 is from a person with acute pancreatitis and shows abnormally high activities of pancreatic fraction. Sample 4 is from a patient with chronic pancreatitis and shows a marked reduction of the pancreatic isoamylase although total serum amylase activity is in the normal range. Sample 5 is from a patient with diabetes mellitus and shows normal exocrine pancreatic function. Sample 6 shows the isoenzyme pattern in serum of a patient with chronic alcoholism and reveals an exocrine pancreatic insufficiency, although total serum amylase activity is the same as in the patient with diabetes mellitus. Sample 7 discloses acute pancreatitis with total serum amylase activity within normal range.
Endoscopic pancreatography.
The fiberduodenoscopes, Olympus JF-B and JF-B2, were used in this series. Sixty per cent Urografin was used for visualization of pancreatic duct. Diagnostic criteria of pancreatogram for pancreatitis are shown in Table 2. From grade of pancreatographic abnormalities, pancreatitis was divided into three groupes, namely minimum, moderate and severe pancreatitis (Fig. 2).
Results and discussion.
Pancreatogram of 18 cases reveals abnormal in 12 cases (66.7%) ; they are 5 minimum, 4 moderate and 3 severe pancreatitis in detail. The remaining 6 cases demonstrate normal pancreatogram (33.3%). Determination of serum pancreatic amylase of 18 cases result 7 (38.9%) low, 2 (11.1%) high and 9 (50.0%) normal activity. Relation between pancreatogram and serum pancreatic amylase activity is shown in Table 4. Pancreatogram and serum pancreatic amylase activity correlate with 11 out of 16 cases (68.7%). This result indicates that if determination of serum pancreatic amylase activity were used for screening test of pancreatitis, there would be 40% of false negative. But this method is easy and simple compared to pancreozymin-secretin test, and there is no problem to repeat the examination, If once low amylase level were found, chronic pancreatitis should be suspected. Rate of correlation of pancreatic amylase activity with pancreatogram is almost the same as that of pancreozymin-secretin test and this method could be recommended.
Relation between abnormal pancreatogram and year of alcoholism is shown in Table 5. Pancreatogram of 15 cases with history of alcoholism of more than 5 years and with delirium tremens reveals normal in 4 cases (26.7%) and abnormal in 11 cases (73.3%). In another way, 11 out of 12 cases with abnormal pancreatogram (91.7%) have history of alcoholism of more than 5 years. Various authors reported that alcohol and low protein diet make fatty degeneration and interstitial fibrosis of pancreatic tissue. It could be imagined that 5 years of heavy drinking and low nutrition result in rather strong histological changes in the pancreas which could be demonstrated even by pancreatography.
Pancreatic calcification and chronic relapsing pancreatitis are frequent in alcoholic pancreatitis. In this series, there were 6 cases (33.3 %) of pancreatic calcification and 9 cases (50.0%) of chronic relapsing pancreatitis.
Summary
1) Endoscopic pancreatography and determination of serum pancreatic amylase activity were performed on 18 cases of chronic alcoholism in Malmo General Hospital, Sweden.
2) Pancreatogram revealed abnormal in 66.7%.
3) Serum pancreatic amylase activity resulted low in 38.9%, high in 11.1% and normal in 50.0%.
4) Correlation of endoscopic pancreatography with serum pancreatic amylase activity is 68.7%.
5) Pancreatogram of patient with history of chronic alcoholism more than 5 years demonstrated abnormal in 73.3%.
6) Pancreatic calcification was observed in 33.3%.
7) Fifty per cent of patients had chronic relapsing pancreatitis, and pancreatogram was abnormal in 77.8%.
Copyright © 1974, Igaku-Shoin Ltd. All rights reserved.


