Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
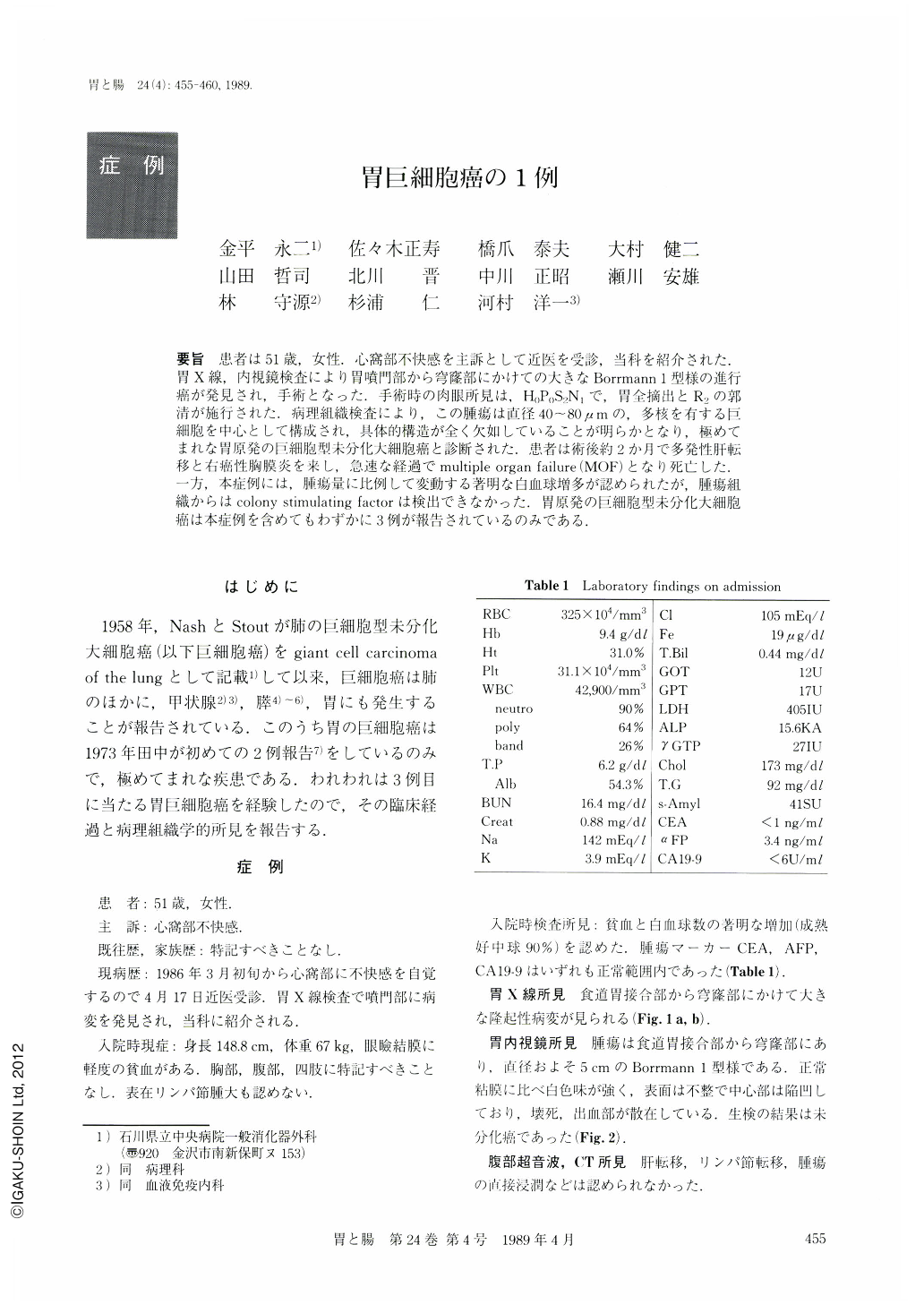
要旨 患者は51歳,女性.心窩部不快感を主訴として近医を受診,当科を紹介された.胃X線内視鏡検査により胃噴門部から穹窿部にかけての大きなBorrmann 1型様の進行癌が発見され,手術となった.手術時の肉眼所見は,H0P0S2N1で,胃全摘出とR2の郭清が施行された.病理組織検査により,この腫瘍は直径40~80μmの,多核を有する巨細胞を中心として構成され,具体的構造が全く欠如していることが明らかとなり,極めてまれな胃原発の巨細胞型未分化大細胞癌と診断された.患者は術後約2か月で多発性肝転移と右癌性胸膜炎を来し,急速な経過でmultiple organ failure(MOF)となり死亡した.一方,本症例には,腫瘍量に比例して変動する著明な白血球増多が認められたが,腫瘍組織からはcolony stimulating factorは検出できなかった.胃原発の巨細胞型未分化大細胞癌は本症例を含めてもわずかに3例が報告されているのみである.
The patient, a 51-year-old female was referred to our hospital because of epigastric discomfort. Upper gastrointestinal series and gastric endoscopy revealed a large Borrmann's Type-1 tumor extending from the cardia to the fornix (Figs. 1 a, 1 b and 2).
Since the operative findings indicated “H0P0S2N1”, total gastrectomy with R2-lymph node dissection was carried out.
Histological findings revealed that the tumor was composed mainly of mufti-nucleated giant cells ranging from 40 to 80 μm in diameter, without any cellular differentiation. Stains for mucin were negative. This histological study led to a diagnosis of giant cell carcinoma of the stomach (Figs. 3 and 4).
The patient, however, began to suffer from multiple liver metastasis and carcinomatous pleuritis only two months after the operation. This was followed by multiple organ failure and rapid deterioration culminating in death.
Another factor in this case was the presence of marked leukocytosis which varied in direct proportion to the volume of the tumor. However, no “colony stimulating factor” could be detected from the tumor tissue.
Up to now, only three cases, including ours, have been reported as giant cell carcinoma of the stomach.
Copyright © 1989, Igaku-Shoin Ltd. All rights reserved.


