Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
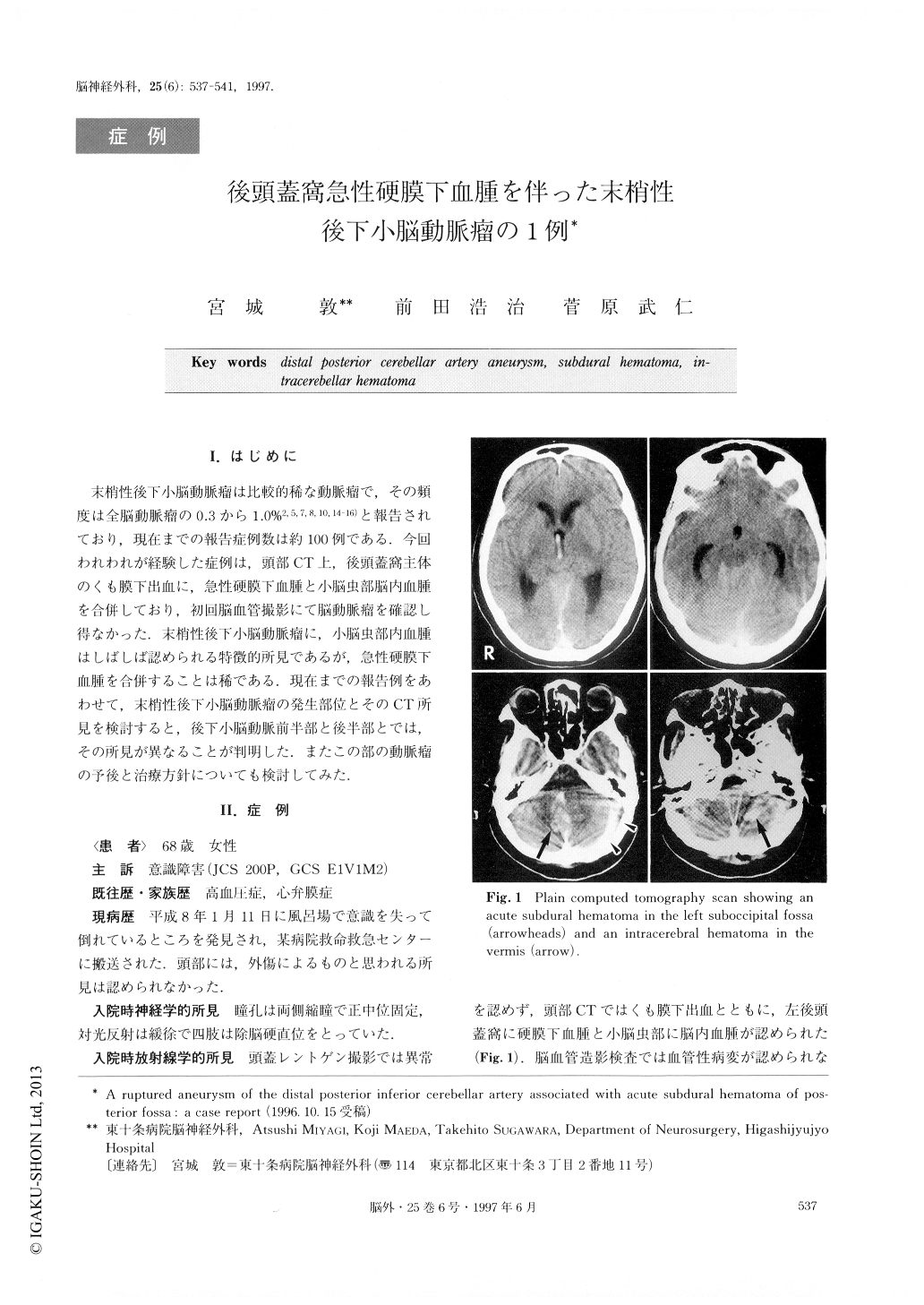
末梢性後下小脳動脈瘤は比較的稀な動脈瘤で,その頻度は全脳動脈瘤の0.3から1.0%2,5,7,8,10,14-16)と報告されており,現在までの報告症例数は約100例である.今回われわれが経験した症例は,頭部CT上,後頭蓋窩主体のくも膜下出血に,急性硬膜下血腫と小脳虫部脳内血腫を合併しており,初回脳血管撮影にて脳動脈瘤を確認し得なかった.末梢性後下小脳動脈瘤に,小脳虫部内血腫はしばしば認められる特徴的所見であるが,急性硬膜下血腫を合併することは稀である.現在までの報告例をあわせて,末梢性後下小脳動脈瘤の発生部位とそのCT所見を検討すると,後下小脳動脈前半部と後半部とでは,その所見が異なることが判明した.またこの部の動脈瘤の予後と治療方針についても検討してみた.
We report a case of distal posterior inferior cerebellar artery (PICA) aneurysm associated with acute subdural hematoma (SDH). The patient was a 68-year-old female who was found unconscious at home and trans-ferred to the emergency medical center in a state of deep coma. Her consciousness on admission to the cen-ter was 200P (Japan coma scale), E1V1M2 (Glasgow Coma Scale), and the Hunt & Kosnik grade was grade Ⅳ. She was in a state of decerebrate condition. Com-puted tomography (CT) scans revealed diffuse subarach-noid hemorrhage that was located mainly in the pos-terior fossa, as well as intraventricular hemorrhage in the third and fourth ventricles. It also disclosed an in-tracerebellar hematoma (ICH) of the vermis and an acute SDH of the left posterior fossa. The first cerebral angiographic examinations on admission demonstrated no aneurysm. However, emergency surgery was per-formed immediately in order to improve her poor con-dition. Ventricular drainage and removal of the acute SDH were carried out. Postoperatively, her conscious-ness improved gradually to 20P. Ventricular peritoneal shunt was performed three weeks later. Her conscious-ness improved up to 3P and she showed only slight truncal ataxia. She was admitted to our hospital for re-habilitation at two months after the first surgery. Re-peated angiography was performed and demonstrated an aneurysm in the telovelotonsillar segment of the left PICA. The aneurysm was successfully clipped via a midline suboccipital approach. Her postoperative course was uneventful, and she continues to undergo rehabi-litation. Aneurysms of the posterior fossa associated with acute SDH are extremly rare. Only two cases have been reported for distal PICA aneurysm cases. The CT scans in our patient revealed not only SAH but also SDH in the posterior fossa and ICH in the ver-mis. Over 100 cases of distal PICA aneurysms have been described in the literature. We analyzed the rela-tionship between the portions with the ruptured aneurysms and CT findings. Aneurysms which were lo-cated at the proximal portion of the distal PICA mainly showed SAH and IVH. On the other hand, ICHs of the vermis and cerebellum were characteristic CT findings of ruptured aneurysms which were located more distal to the telovelotonsillar segment, and were evident in 14% of cases of such aneurysms. ICH and SDH were not found in aneurysms which were located in portions more proximal to the telovelotonsillar segment. These characteristic findings were related to the complex ana-tomical courses of the PICA. The distal portions of the PICA run between the vermis and cerebellar hemi-sphere, so that if an aneurysm ruptures at these por-tions, ICHs in the vermis and cerebellum tend to occur. In cases such as ours, because of the characteristic CT findings, effort to detect a distal PICA aneurysm should be made at first surgery, along with ventricular drainage and removal of the SDH. The surgical proce-dures and outcome of cases with distal PICA aneu-rysms are also discussed.
Copyright © 1997, Igaku-Shoin Ltd. All rights reserved.


