Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
脳神経外科領域で手術支援を目的とした画像誘導装置が開発されてから間もないが,画像診断とコンピュータの進歩によりその精度や操作性は年々改善され,数種類が実用化されている.われわれの施設でも1995年度よりカナダISG社製のViewing Wand®が導入され,実際の手術に応用している.まだ症例数は少ないが,この装置を用いた難治性てんかんの手術例を提示し,画像誘尊手術の利点,問題点について報告する.
Availability of a neuronavigation system for epilepsy surgery was reported, and its practical use was dis-cussed.
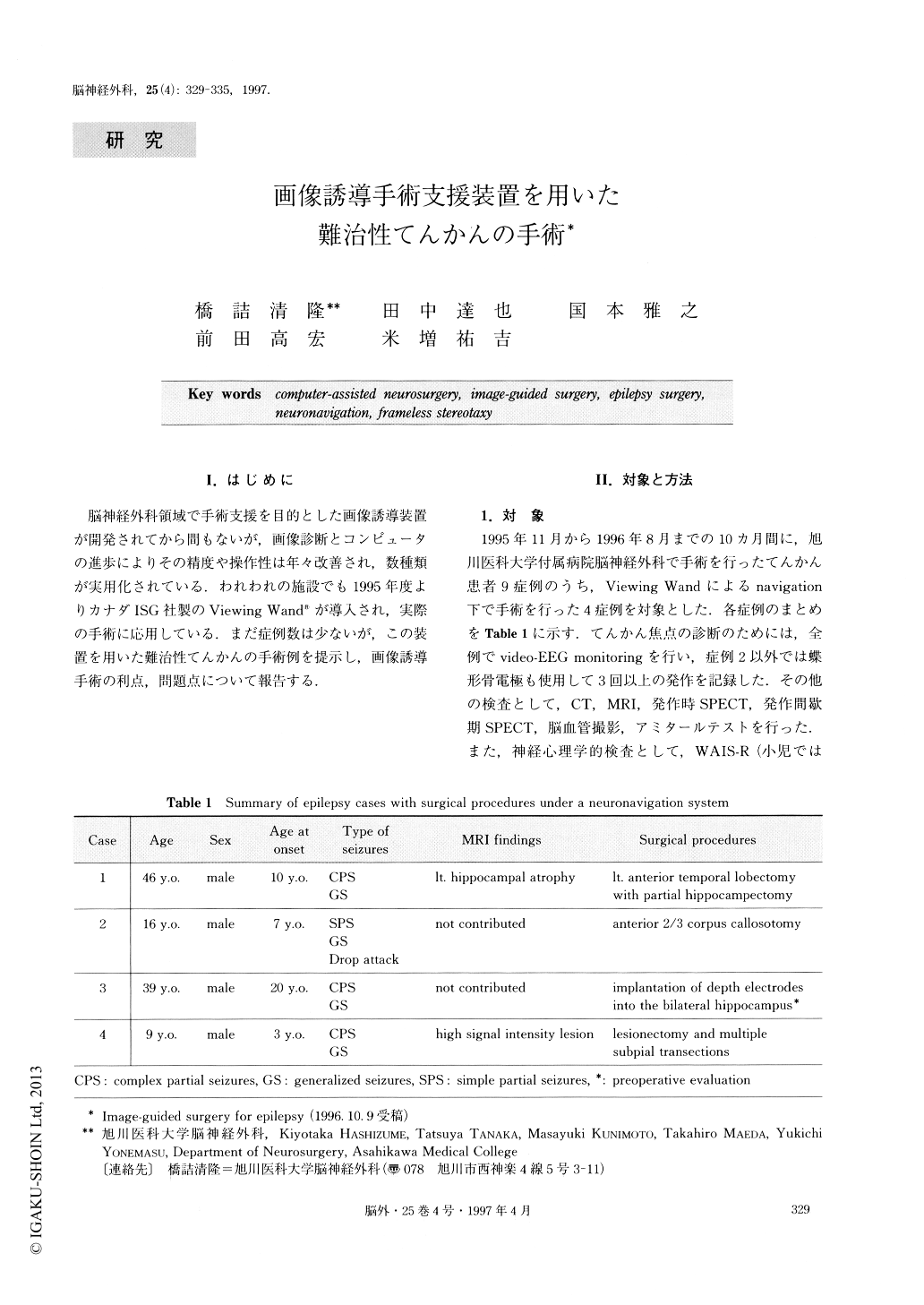
Four of nine patients with intractable epilepsy under-went surgical procedures using a neuronavigation sys-tem, Viewing Wand ® , from November 1995 to August 1996, in our hospital. The ages of patients were be-tween 9 to 46 years old. Three of them had temporal lobe epilepsy and one had generalized tonic seizures. One of the temporal lobe epilepsy cases had focal cor-tical dysplasia in the left posterior temporal lobe, and the other one showed left hippocampal atrophy on MR images. The remaining two patients had no abnormal-ity on MR images. All patients underwent video-EEG monitoring and habitual seizures were recorded at least three times. Ictal and/or interictal SPECT and neuro-psychological testing were also performed. Electrocor-ticograms were recorded intraoperatively in all patients. Surgical procedures using the neuronavigation system were anterior temporal lobectomy, corpus callosotomy and lesionectomy of focal cortical dysplasia. A patient with temporal lobe epilepsy underwent implantation of depth electrodes under the neuronavigation. In temporal lobectomy, image-guided surgery helped to make a decision concerning the safely-resectable size of the lateral temporal cortex and hippocampus. The hippocampus was resected with minimum surgical dam-age and it made possible a complete histopathological examination. In corpus callosotomy, although it was not easy to confirm the length of the callosal section, the neuronavigation system enabled this to be done quickly. The real-time navigation showed the accurate operating position on three-dimensional images. The location of focal cortical dysplasia was often difficult to identify macroscopically. However, the location of the lesion can be projected to the skin surface under the neuronavigation system. The width of skin incision and craniotomy was able to be made smaller, and the surgery was able to be performed less invasively. The Viewing Wand system was accurate, reliable and easy to operate in these procedures. The navigat-ing error was 2-5mm. Using CT image data of 5mm thickness the error was greater, although use of MR image data of 2mm thickness resulted in relatively small error up to 2-3mm. The first major factor of the error was the fiducial registration of the patient's head. While the registration was made more strictly with multiple fiducial points, the error was smaller. The second factor was movement of patient's head and/or the navigation arm. The arm and the head should be fixed tightly to the operating table, and it is better if they are fixed together with a supporting arm. The third factor was intraoperative brain shift caused by flow out of the cerebrospinal fluid or removal of mass lesions. This type of error is common in all navigation systems. However, it may be avoided making some real-time feedback system. With the Viewing Wand system, repetition of the intraoperative registration us-ing intracranial anatomical structures reduces this type of error. On the other hand, there were some difficul-ties on stereotaxic procedures, such as implantation of depth electrodes, using the Viewing Wand. The error was larger than that recorded in other frame-based stereotaxic apparatus. This problem may be improved by a supporting system to fix the probe position. As a neuronavigation system can be widely applied to neuro-surgical procedures, we consider that epilepsy and skull-base surgery are the best targets for it because of the minimum possible brain shift. We hope that accu-rate and less-invasive surgery using a neuronavigation system will contribute to a better outcome for epilepsy patients.
Copyright © 1997, Igaku-Shoin Ltd. All rights reserved.


