Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
近年,巨大脳動静脈奇形(以下AVM)の治療は手術を考慮した場合,手術前に段階的に塞栓術を行うことが一般化されつつあり,それに伴い塞栓術に固有な合併症に対する認識の必要性も増してきたと思われる.今回,われわれは左後頭葉巨大動静脈奇形に対し,手術前に椎骨脳底動脈経由で塞栓術を試みた際に高度のクモ膜下出血および橋出血を発症した例を経験したので,AVM塞栓術の出血性偶発症について文献的に考察する.
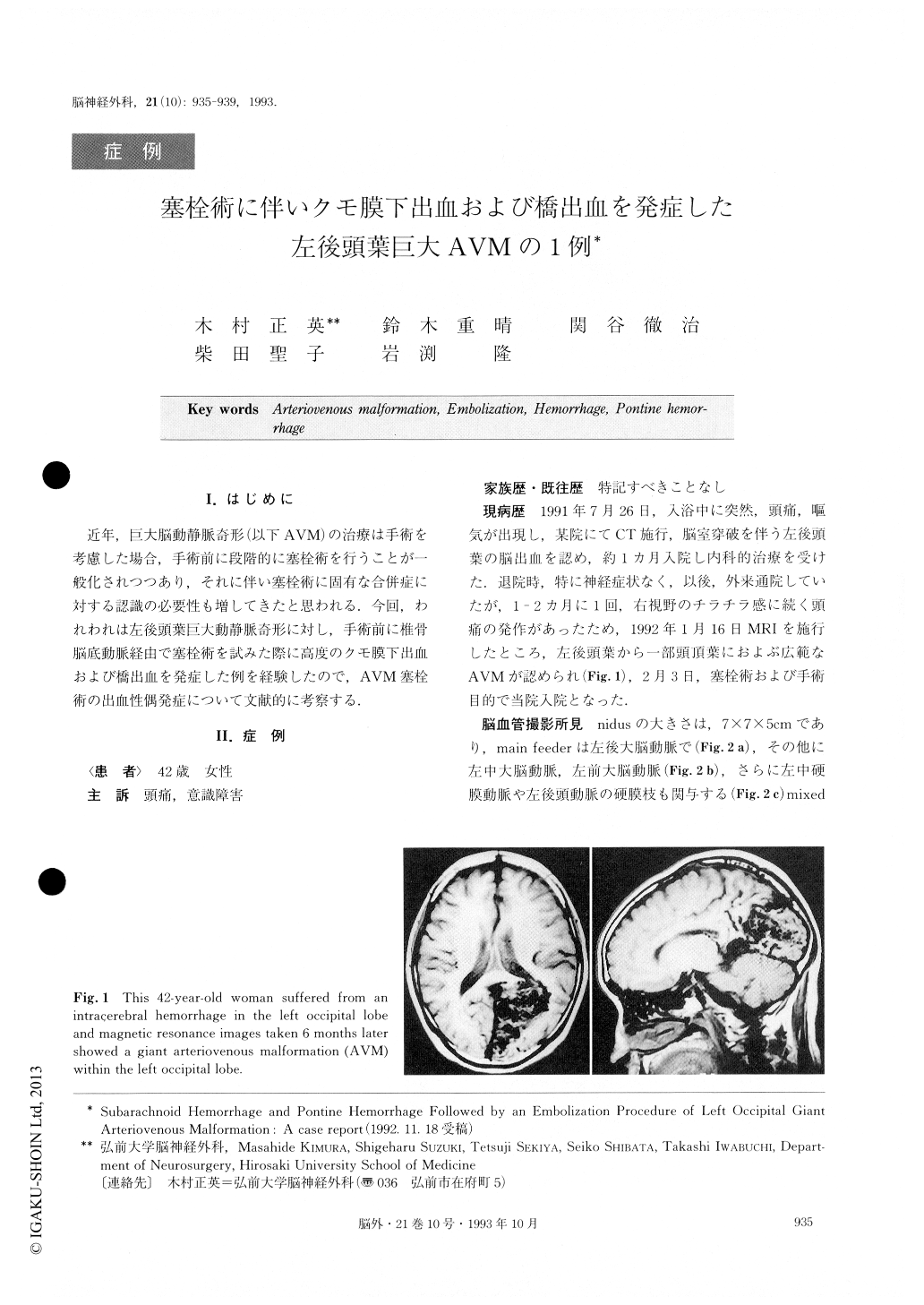
A 42-year-old woman suddenly developed headacheand nausea on July 26, 1991, and the computed tomogra-phy (CT) scan showed a moderate-sized hematoma in the left occipital lobe. After one month's conservative treatment, she had recovered to a neurologically intact state.
Cerebral angiography demonstrated a giant arteriove-nous malformation fed by enlarged branches of the left posterior cerebral artery as well as small branches aris-ing from the middle cerebral artery, anterior cerebral artery and the meningeal branches of the middle menin-geal artery and the occipital artery. Preoperative embo-lization was planned on February 24, 1992. During an attempt at catheterization of the basilar artery and the left posterior cerebral artery with a balloon catheter and a Tracker-18 catheter, the patient complained of an in-tensification of her headache, nausea and vomiting. So the embolization procedure was stopped. The CT scan taken immediately at that time showed a severe sub-arachnoid hemorrhage (SAH). She became comatose ab-out 40 minutes later. CT scan taken next day revealed also a complication of the pontine hemorrhage.
Neurologically, she had gradually recovered and could communicate with some simple words 3 months after SAH. The total removal of the AVM was performed on May 26, 1992. Postoperative course was uneventful. She showed rapid and remarkable improvement in her neuro-logical state suggesting that the blood flow in the sur-rounding brain area had been corrected. A blood deficit had no doubt been caused when blood had been stolen by the giant AVM.
In recent literature, the incidence of hemorrhagic com-plications of embolization is reported to be 4 - 11%, and two types of hemorrhage have been identified ; immedi-ate SAH caused by perforation or rupture of the feeding artery during the catheterization process, and delayed in-tracerebral hemorrhage due to the rupture of the partial-ly embolized AVM. We suppose that SAH in our case was caused by the former mechanism. However, pontine hemorrhage, which was located in an area remote from the occipital AVM, may have occurred secondarily by some other mechanism after the abrupt and severe SAH.
Copyright © 1993, Igaku-Shoin Ltd. All rights reserved.


