Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
急性あるいは慢性難治性うっ血性心不全患者では,しばしば著明な肺うっ血とともに低心拍出量状態に対応して,体血管抵抗と静脈緊張が代償的に増加する。このような左室流出路インピーダンスの増加と左室終末弛期圧の上昇は,左室張力の増しから心筋酸素消費量を増大させ,結果的にきわめて不利な状態をもたらす1〜4)。急性左室不全あるいは急性肺水腫に対する後負荷や前負荷の軽減療法の試みは,自律経神節遮断剤の臨床導入以来,しばしば行なわれ,急性症状の改善に好結果をえた5〜7)。しかし,重症慢性左室不全に長期的かつ効果的な負荷軽減療法が行なわれるようになったのは,近年,有効な経口血管拡張薬が広く臨床に応用されるようになってからである。体動脈,または同時に体静脈の血流抵抗を減じ後負荷や前負荷を軽減すれば,左室張力の減少から心筋酸素摂取量の減少を結果し,一方左室駆血が容易に行なわれ,不全心の仕事能を改善し,症状の軽減が期待できる8〜46)。
The effects of oral vasodilators on both resting and exercise hemodynamics were studied in 24 patients with chronic congestive heart failure. Vasodilators included prazosin (PZ), isosorbide dinitrate (ID) and hydralazine (HD).
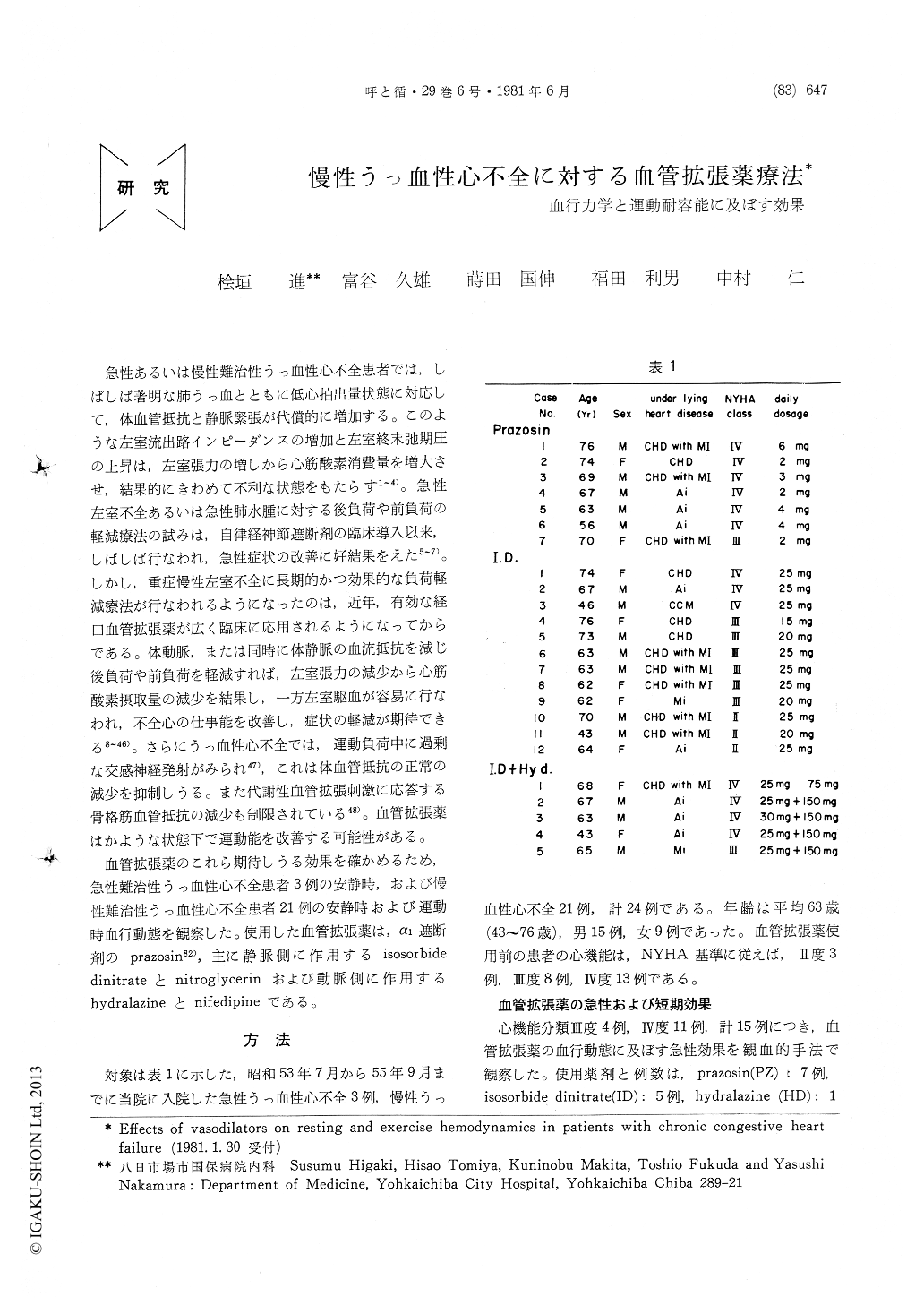
Significant hemodynamic responses to 0.5 to 1.5 mg of prazosin were obtained within one hour, reaching its peak effect during 2 to 4 hours and terminating 6 hours after PZ. Cardiac index (CI) increased markedly from 2.45+0.53 to 3.46±1.18L/min/m2 (p<0.05), together with signifi-cant (p<0.05) increase in stroke index and left ventricular stroke worke index (LVSWI), while systemic vascular resistance (SVR,2302±974 to 1497±614 dynes・sec/cm5), left ventricular filling pressure (LVFP, 24.6+1.4 to 12.8+3.8 mmHg) and mean pulmonary artery pressure (PAm, 34.0 ±4.3 to 19.5±7.0 mmHg) decreased significantly (p<0.01). Mean systemic blood pressure lowered slightly but significantly but heart rate remained unchanged. Such significant first dose effects had been obtained throughout the first 7 days with 2 to 6 mg of constant daily dose of PZ, with remarkable improvement of effort tolerance and exercise hemodynamics determined by a multistage ergometric stress testing in the supine position. Thus, after 7 days short-term PZ therapy, benifical hemodynamic responses were record-ed in patients with refractory congestive heart failure in this series, despite other studies reporting tachphylaxis to higher (5 to 10 mg) serial doses of this drug. The effects of ID were observed within 30 min and continued for 4 hours. Five mg of ID lowered LVFP (22.8+±.0 to 14.9 ±3.9 mmHg, p<0.01) and PAm (33.5±6.1 to 22.4±8.3 mmHg, p<0.001) and improved LVSWI significantly, although increase in CI was not statistically significant. Hydralazine increased in CI and decreased in SVR markedly without any significant changes in LVFP and PAm. Remark-able long-term (3 to 6 months) effects on functional capacity of those vasodilators were observed in 13 out of 18 patients initially showing III or IV of functional capacity.
Copyright © 1981, Igaku-Shoin Ltd. All rights reserved.


