Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
はじめに
早期食道癌はごく最近まで全く報告をみなかったが,1966年東北大山形ら1),東京女子医大中山ら2)の報告以来,各種食道検査法の進歩向上と相俟って次第に多くなってきた,
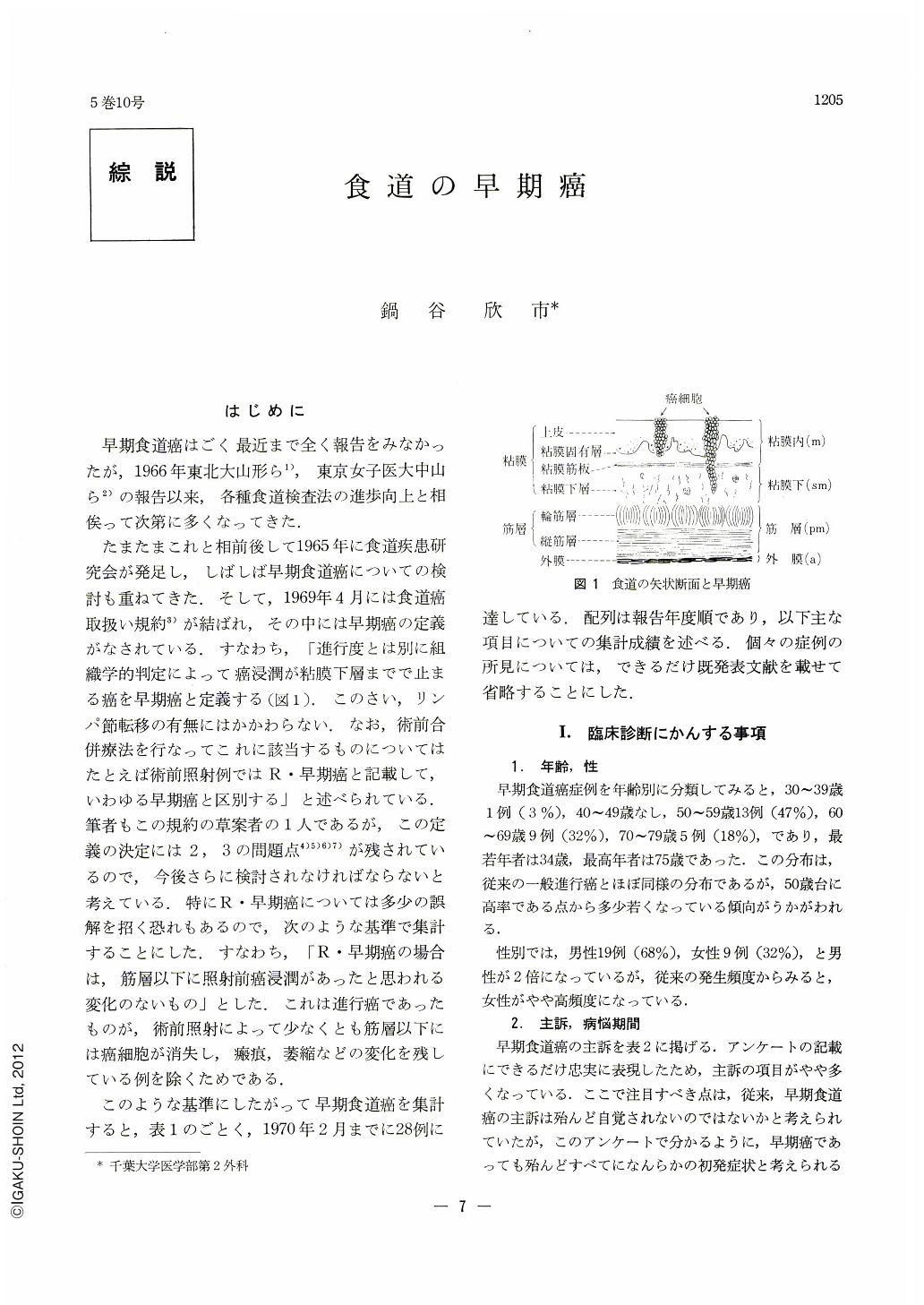
たまたまこれと相前後して1965年に食道疾患研究会が発足し,しばしば早期食道癌についての検討も重ねてきた.そして,1969年4月には食道癌取扱い規約3)が結ばれ,その中には早期癌の定義がなされている.すなわち,「進行度とは別に組織学的判定によって癌浸潤が粘膜下層までで止まる癌を早期癌と定義する(図1).このさい,リンパ節転移の有無にはかかわらない.なお,術前合併療法を行なってこれに該当するものについてはたとえば術前照射例ではR・早期癌と記載して,いわゆる早期癌と区別する」と述べられている.筆者もこの規約の草案者の1人であるが,この定義の決定には2,3の問題点4)5)6)7)が残されているので,今後さらに検討されなければならないと考えている.特にR・早期癌については多少の誤解を招く恐れもあるので,次のような基準で集計することにした.すなわち,「R・早期癌の場合は,筋層以下に照射前癌浸潤があったと思われる変化のないもの」とした.これは進行癌であったものが,術前照射によって少なくとも筋層以下には癌細胞が消失し,瘢痕,萎縮などの変化を残している例を除くためである.
このような基準にしたがって早期食道癌を集計すると,表1のごとく,1970年2月までに28例に達している.配列は報告年度順であり,以下主な項目についての集計成績を述べる.個々の症例の所見については,できるだけ既発表文献を載せて省略することにした.
Early esophageal cancer is defined as carcinomatous lesion of the esophagus with its infiltration limited within the submucosal layer regardless of the presence or absence of lymph node metastasis. It is further stated that early esophageal carcinoma receiving preoperative irradiation should be named as “R-early carcinoma” as distinguished from nonirradiated early carcinoma. However, since this division still contains many controversial points, the R-early carcinoma in this paper is limited to esophageal cancer in which carcinomatous infiltration can not have reached the musclar coat before irradiation. This distinction has been adopted to rule out those advanced carcinomas in which cancer cells have disappeared at least in or beyond the musclar coat by preoperative irradiation, leaving evidence of cicatrization or atrophy there.
The progress in various diagnostic methods has enabled us to diagnose carcinoma of the esophagus in its early stage. Thus 28 cases of early esophageal carcinoma have been reported in Japan. They include 19 males and 9 females. The age ranged from 34 to 75 years with the greatest incidence between 50 and 59 years.
The chief complaints are, in many instances, retrosternal pain, dysbhagia and/or unusual feeling upon swallowing. The complaints are often of short duration of 2~3 months.
As for the site of the lesion, it was in the cervical portion in 4, the upper thoracic portion in 3, the middle thoracic portion in 14, and the lower thoracic portion in 7, showing higher incidence in the middle and lower thoracic portions. They were all squamous cell carcinomas histologically.
As for the radiographical configuration, it was tumor type in 15, superficial type in 6, and serrated type in 5, while uncertain in 2 cases.
Endoscopy was performed in 25 cases, in which the lesion was of superficial type in 21, elevated type in 1, depressed type in 2 and uncertain in 1.
Biopsy and cytology were carried out in 21 cases, all of which were preoperatively correctly diagnosed as of carcinoma except in one case which was diagnosed as a benign tumor. This illustrates high accuracy of this method of diagnosis.
The examination with 32P, performed in 3 cases, made it possible to diagnose an extremely small carcinoma. Therefore, the above-mentioned various methods should be combined for accurate diagnosis.
The lesions were all within 4cm in diameter except one which was a surface-expanding type of more than 6cm in diameter. The grade of depth extension was intramucosal (m) in 3 submucosal (sm) in the other 25 cases.
The operative technique varied in different institutions, but the direct operative mortality was only one in 28 cases (3%).
The long-term results are much better than those of advanced carcinomas. However, one patient showed intravascular infiltration even in the early stage, dying of a recurrence. Furthermore, there were 3 early postoperative deaths, indicating difficulty in the postoperative care.
Copyright © 1970, Igaku-Shoin Ltd. All rights reserved.


