Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
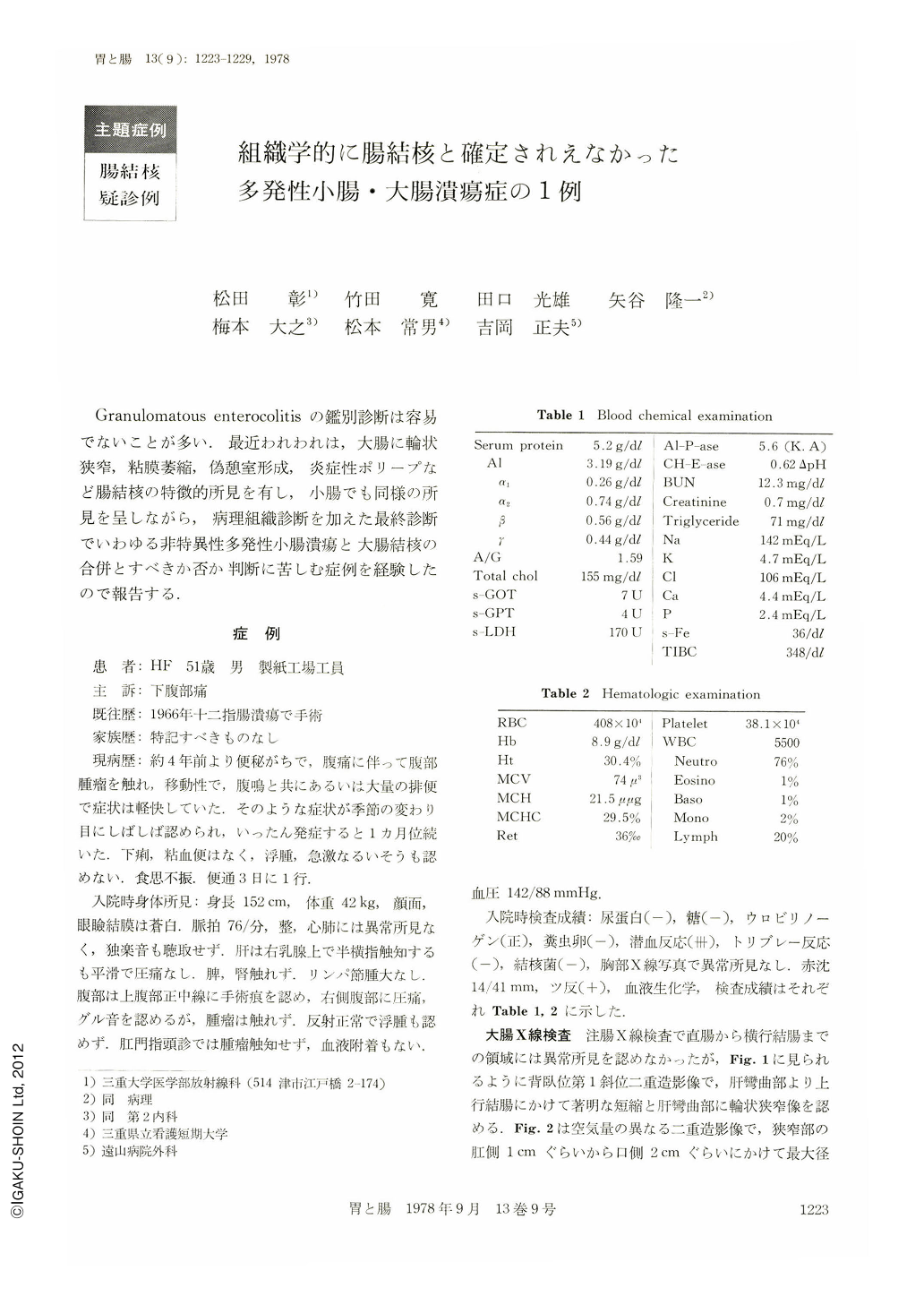
Granulomatous enterocolitisの鑑別診断は容易でないことが多い.最近われわれは,大腸に輪状狭窄,粘膜萎縮,偽憩室形成,炎症性ポリープなど腸結核の特徴的所見を有し,小腸でも同様の所見を呈しながら,病理組織診断を加えた最終診断でいわゆる非特異性多発性小腸潰瘍と大腸結核の合併とすべきか否か判断に苦しむ症例を経験したので報告する.
症 例
患 者:HF 51歳 男 製紙工場工員
主 訴:下腹部痛
既往歴:1966年十二指腸潰瘍で手術
家族歴:特記すべきものなし
現病歴:約4年前より便秘がちで,腹痛に伴って腹部腫瘤を触れ,移動性で,腹鳴と共にあるいは大量の排便で症状は軽快していた.そのような症状が季節の変わり目にしばしば認められ,いったん発症すると1カ月位続いた.下痢,粘血便はなく,浮腫,急激なるいそうも認めない.食思不振 便通3日に1行.
A 51-year-old man was admitted to Toyama Hospital complaining of periodic episodes of lower abdominal pain for four years. He had anemia and hypoproteinemia.
Stool examination for occult blood was strongly positive. Cultures of stool for tubercle bacillus were negative and there were no abnormal findings in the chest roentgenogram.
Double contrast radiogram of gastrointestinal tract showed girdle ulcers, circular narrowings and inflammatory polyps in the ileum and circular narrowing, atrophic mucosa, pseudodiverticuli and multiple ulcer scars in the ascending colon.
These X-ray findings strongly suggested intestinal tuberculosis. Partial ileocolectomy was performed.
The resected specimen showed multiple girdle, rounded, or irregular-shaped ulcers in the lower ileum and narrowing, shortening with atrophic mucosa and healed ulcers in the ascending colon, The terminal ileum measuring about 30 cm in length had no ulcerative lesions.
Histologically, the ulcers of the ileum were confined within the submucosa (Ul-Ⅱ) and no evidence of specific granulomatous changes was obtained in these lesions.
There were also no proliferative mucosal changes among the ulcers. It was therefore thought that the ileal lesions were consistent with the so-called non-specific multiple ulcers of the small intestine proposed by Okabe and Yao.
On the other hand, in the ascending colon, some epitheloid cell granulomas were observed in the submucosa but no tendency to caseation necrosis was seen. Therefore, the final histological diagnosis of this lesion could not be made in spite of its typical macroscopic apearance of tuberculosis. Shirakabe reported that the difference between macroscopic (including X-ray) findings and histological appearance depended upon the process of the lesion, and he emphasized the superiority of the macroscopic pictures in diagnosing intestinal tuberculosis.
According to his statement, this lesion might be consistent with tuberculosis. However, histologically it might be diagnosed as non-specific granulomatous colitis.
We thought there might be two ways to interprete the findings of this case. It was as follows; (1) tuberculosis of the ascending colon complicated with non-specific multiple ulcers of the ileum.
(2) non-specific inflammatory changes both in the large and small intestine.
Copyright © 1978, Igaku-Shoin Ltd. All rights reserved.


