Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- 参考文献 Reference
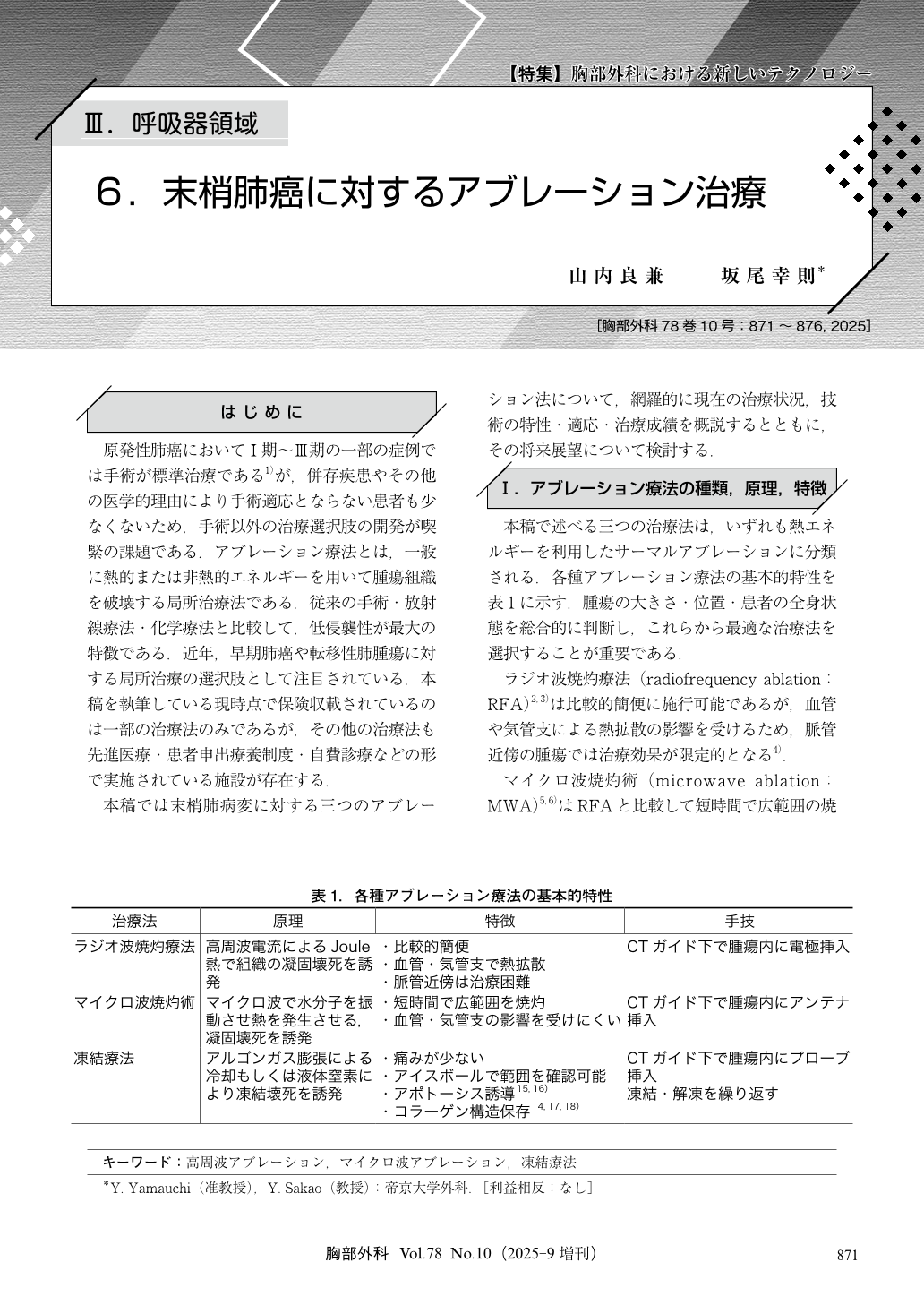
原発性肺癌においてⅠ期~Ⅲ期の一部の症例では手術が標準治療である1)が,併存疾患やその他の医学的理由により手術適応とならない患者も少なくないため,手術以外の治療選択肢の開発が喫緊の課題である.アブレーション療法とは,一般に熱的または非熱的エネルギーを用いて腫瘍組織を破壊する局所治療法である.従来の手術・放射線療法・化学療法と比較して,低侵襲性が最大の特徴である.近年,早期肺癌や転移性肺腫瘍に対する局所治療の選択肢として注目されている.本稿を執筆している現時点で保険収載されているのは一部の治療法のみであるが,その他の治療法も先進医療・患者申出療養制度・自費診療などの形で実施されている施設が存在する.
Ablation therapy is a minimally invasive local treatment that destroys tumor tissue. It has attracted attention as a treatment option for early-stage lung cancer and metastatic lung tumors. In this review, we provide an overview of the current status of treatment, technical characteristics, indications, and treatment results for three ablation methods for peripheral lung lesions:radiofrequency ablation (RFA), microwave ablation (MWA), and cryoablation (PCT). RFA is relatively simple to perform, but its therapeutic effect is limited in tumors near blood vessels due to the influence of heat diffusion by blood vessels and bronchi. MWA enables wide-range ablation in a short time compared to RFA and has the advantage of being less affected by blood vessels and bronchi. PCT enables easy confirmation of the ablation range because it can be visualized as an ice ball on computed tomography (CT) fluoroscopy and is less painful for the patient. It is characterized by the induction of tumor cell death by apoptosis and the preservation of tissue structure. The indications for ablation therapy are mainly early-stage non-small cell lung cancer (NSCLC) that is difficult to surgically resect. Patients with high surgical risk, such as elderly patients and patients with serious complications, are targeted. The combination of ablation therapy and immunotherapy is expected to have a therapeutic effect, and systemic antitumor effects through the release of tumor-associated antigens can be expected. In the future, further expansion of treatment options for lung cancer is expected with the development of optimal combination methods with immunotherapy and the development of transbronchial approaches.
© Nankodo Co., Ltd., 2025


