Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
後頭蓋窩硬膜動静脈奇形(dural arteriovenous malfor—mation,以下dural AVM)は,Newton12)が“dural arte—riovenous malformation in the posterior fossa”として報告して以来,診断技術の進歩に伴い多くの報告がみられるようになって来た.しかしその発生機序に関しては先天的に存在していた動静脈吻合が発達したとする先天説と,外傷や静脈洞血栓により後天的に発生したとする後天説の2つの考え方があり,未だ結論を見ていない.また治療法に関しても外科的摘出術やembolizationなどが行われているが,現在も議論を呼ぶところである.
最近われわれは,浅側頭動脈—中大脳動脈(STA—MCA)吻合術を施行後,外頸動脈系の拡張とともにdu—ral AVMが出現した症例を経験したので,特にその発生機序について,文献的考察を加えて報告する.
A case of dural arteriovenous malformation (AVM) in the posterior cranial fossa detected after STA-MCA anastomosis surgery.
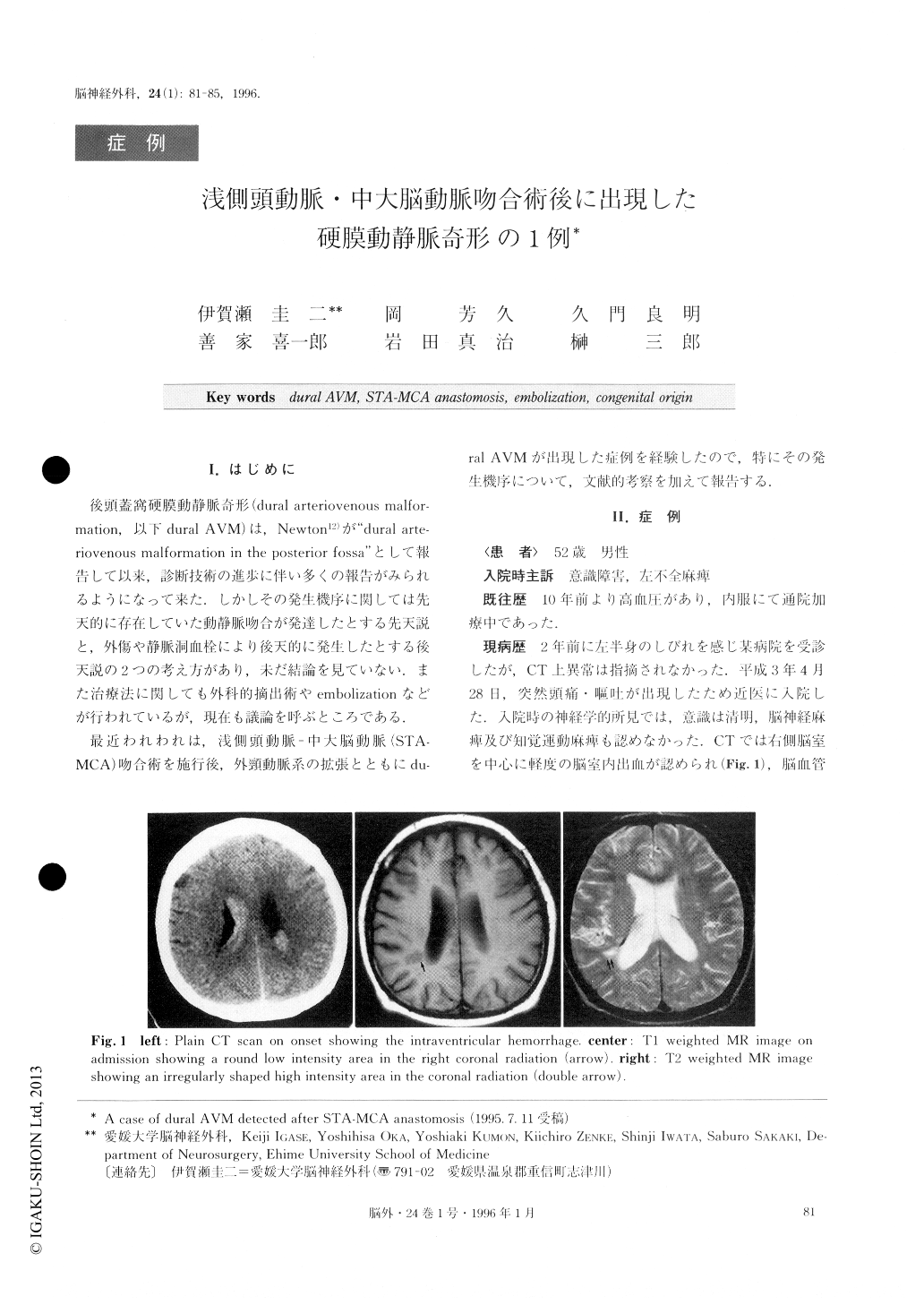
A 52-year-old male consulted a neighbourhood hos-pital for sudden headache and vomiting. He was dia-gnosed as having intraventricular hemorrhage on CT scan. Though the obstruction of the right internal caro-tid artery was revealed angiographically, his symptoms improved after conservative therapy. Two weeks after onset, his consciousness deteriorated and he developed left hemiparesis. Thereafter, he was transferred to our hospital. After thorough examination, right STA-MCA anastomosis surgery was performed. Approximately 2 months after surgery, right tinnitus developed and gra-dually exacerbated. Since it was thought to be due to increased blood flow in the right superficial temporal artery, it was kept under observation. On angiogram, 8 months after surgery, good blood flow supplied from the right superficial temporal artery to the territory of the right middle cerebral artery was shown, and a dural AVM fed by the right occipital artery was found.
Fourteen months after the surgery, an enlarged dural AVM with backflow to the superficial cerebral veins fed by the enlarged right occipital artery and right ascending pharyngeal artery was revealed. Emboliza-tion therapy to the right occipital and ascending pharyn-geal artery was performed using coils and ivalon, and irradiation of 30 Cry was added. After this treatment, right tinnitus improved. On angiography 2 years later, transverse sinus was slightly visible via the right occi-pital artery and ascending pharyngeal artery, but the dural AVM was significantly reduced.
The origin of dural AVMs remains controversial. In our case, dural AVM was not found before the STA-MCA anastomosis surgery, and sinus thrombosis was not found throughout the course of observation. It is thought that the occult dural AVM was disclosed and enlarged by the increased blood flow through the exter-nal carotid artery via the STA-MCA anastomosis. Therefore, the dural AVM seemed to be congenital in origin.
Copyright © 1996, Igaku-Shoin Ltd. All rights reserved.


