Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
脳血管奇形(cerebrovascular malformation:CVM)は,組織学的に,arteriovenous malformation(AVM),cavernous angioma, venous angiomaおよびcapillary telangiectasiaの4型に分類されてきた10).しかし,これらの4型のいずれに分.類すべきか困難であったり,同一症例で2つ以上のCVMが隣接して認められたとする報告が散見される1,6-8,11,13).われわれはいわゆるve—nous angiomaと他のCVMの存在が確認された3症例を報告し,同一症例において,venous angiomaと他のCVMが併存する意義および,このような症例の治療法について考察する.
The authors report 3 cases in which, in addition to venous angioma, other types of vascular malformations coexisted. They discussed the pathological significance of this coexistence, and the treatment to be given in these conditions.
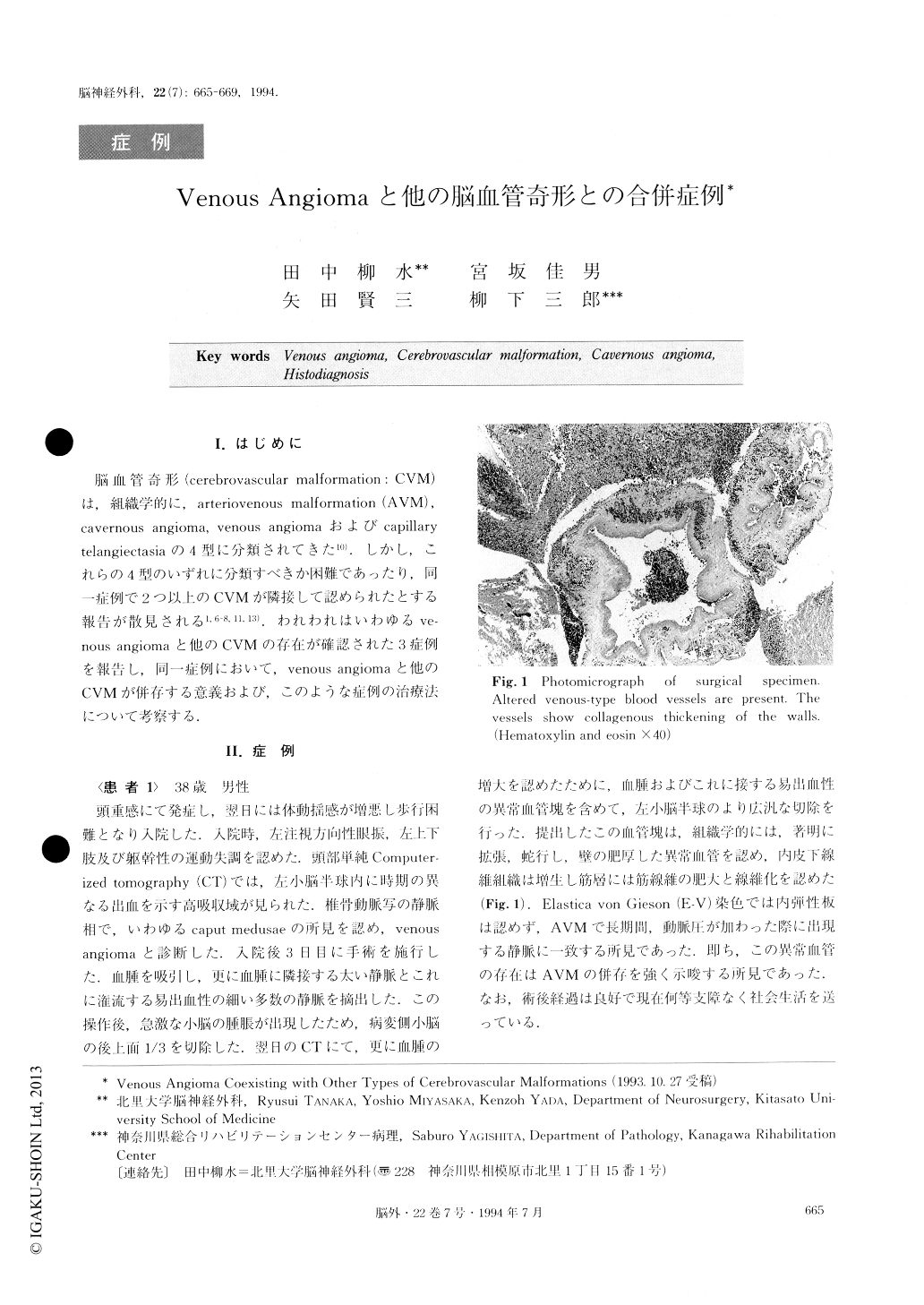
Case 1: A 38-year-old man was admitted to the hos-pital because of progressive headaches of 3 days' dura-tion. X-ray CT revealed a large hematoma in the left cerebellar hemisphere. Vertebral angiogram showed a caput medusae in the venous phase, which is a typical picture of venous angioma. The hematoma was surgi-cally removed and careful inspection of the cavity wall was made. A thick vein and many thin walled dilated venules draining to the vein were observed in the cav-ity wall. These abnormal vessels were completely re-moved. Because of reaccumulation of the hematoma and massive edema of the hemisphere, reoperation was performed. On removing a part of the cerebellar hemi-sphere, a small mass of vascular network was found and removed together with the hematoma.
Histologically, the first specimen was a typical venous angioma, and the second one was a arteriove-nous malformation.
Case 2: A girl 9 years of age was admitted because of headache and left sided ataxia. CT and MRI re-vealed a multi staged hematoma in the left cerebellar hemisphere. Vertebral angiography, however, failed to demonstrate any kind of vascular malformations. The hematoma was removed with its wall. The histological appearance was compatible with venous angioma. 4 years later she bled again, and reoperation was per-formed. Histological examination this time revealed a cavernous angioma.
Case 3: A woman aged 21 years was admitted with intractable convulsive seizures which had continued for 2 years. CT revealed a small calcified lesion in the right frontal lobe. There was no enhanced lesion in the sur-rounding area. Angiogram failed to demonstrate any kind of vascular malformation. Histological examination revealed a cavernous angioma. The second operation was performed because of residue of the lesion found by postoperative CT. The residual area was removed, and histological appearance this time was that of capil-lary telangiectasia. 8 years later, she came back with in-tracerebral hemorrhage at the site of previous lesion. The hematoma with hematoma wall was removed. His-tological examination revealed a venous angioma. Thus, in these 3 cases, in addition to venous angiomas, an AVM, a cavernous angioma, and both a cavernous angioma and capillary telangiectasia were also found. However, venous angioma and cavernous angioma are difficult to differentiate, and there are cases in which the histological picture is intermediate between the typical characteristics of the two, making differentiation so hard that the only identification that can be made is that it is some sort of venous cerebro-vascular malformation.
Copyright © 1994, Igaku-Shoin Ltd. All rights reserved.


