Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
神経鞘腫は硬膜内髄外腫瘍として脊髄腫瘍の約30%を占めるが2),髄内神経鞘腫は稀で現在までに約30例の報告が見られるのみである2,3,9-13,15,21,23).今回われわれはneurofibromatosisを伴わず,胸髄髄内神経鞘腫に頭蓋内多発性髄膜腫を合併した1例を経験したのでここに報告する.
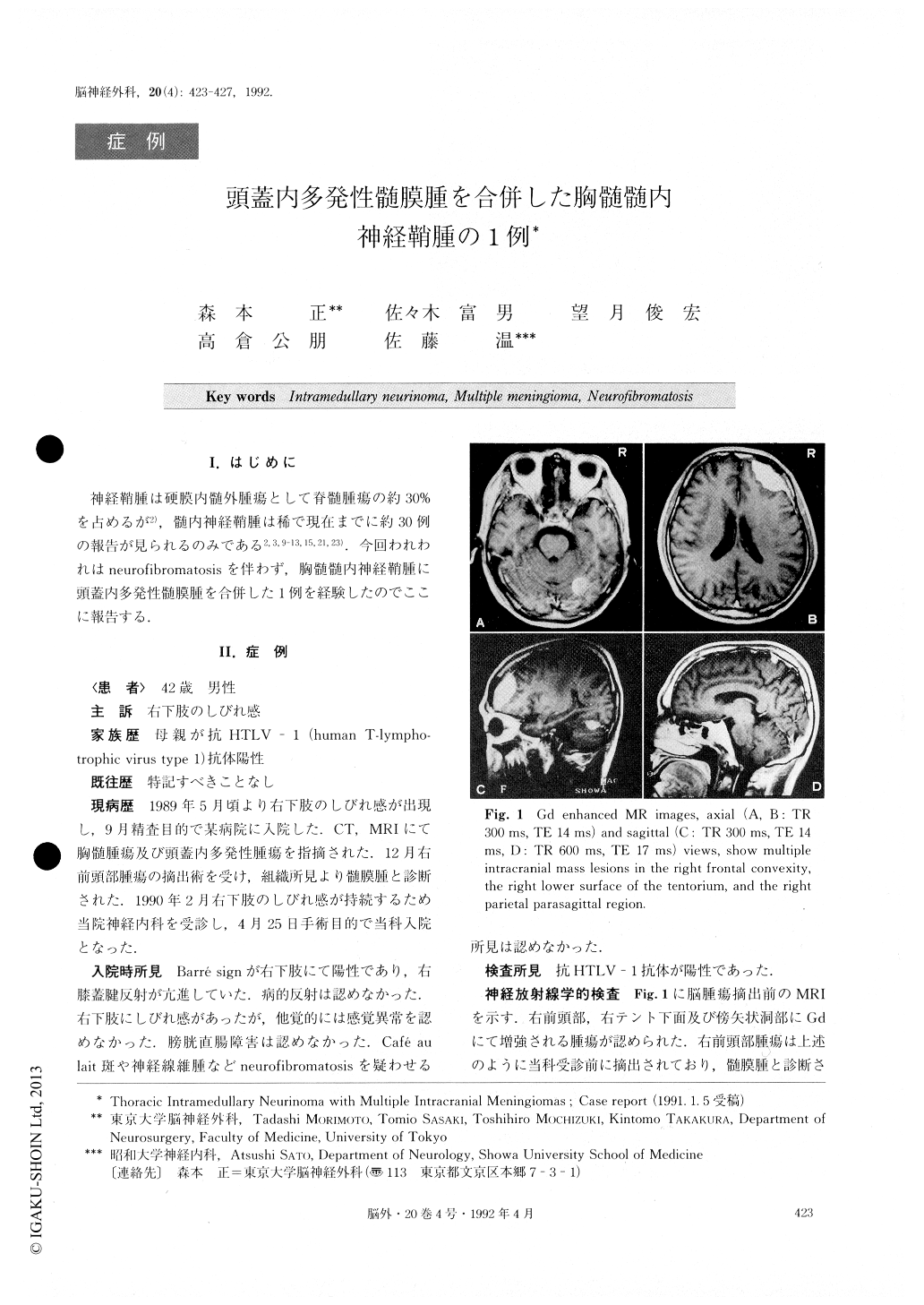
A 42-year-old man suffered from numbness in his right leg in May, 1989, and was admitted to another hospital for examination. Computed tomography and magnetic resonance imaging revealed thoracic in-tramedullary tumor and multiple intracranial tumors in the right frontal convexity, the right lower surface of the tentorium and the right parietal parasagittal region. In December, he underwent craniotomy and the right frontal tumor was totally removed. It was diagnosed histologically as meningioma.
Because of continuing numbness in his right leg, he visited a neurologist at our university and was referred to us for removal of the spinal tumor on April 25, 1990. Neurological examination on admission revealed mild weakness of his right leg and exaggerated right knee jerk. Though he complained of numbness in his right leg, no sensory disturbance was demonstrated objec-tively. His bladder-bowel function was normal. There were no cafe au lait spots or subcutaneous neurofibro-mas. He and his mother were positive for anti-HTLV-1 (human T-lymphotrophic virus type 1) antibody. On May 1, laminectomy was performed at Th-7 to Th-9, and a yellowish brown tumor was found occupying the right posterolateral portion of the cord and extending to the surface. The dorsal root of Th-9, which was in-volved in the tumor, was cut and the tumor was sub-totally removed. Histological examination showed inter-lacing bundles of spindle cells and loose areolar region. Immunohistochemically, the tumor was positive for S-100 protein and negative for GFAP. From these find-ings, the tumor was diagnosed as neurinoma. The post-operative course was uneventful, numbness dis-appeared, and the patient was discharged without neurological deficits.
Copyright © 1992, Igaku-Shoin Ltd. All rights reserved.


