Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
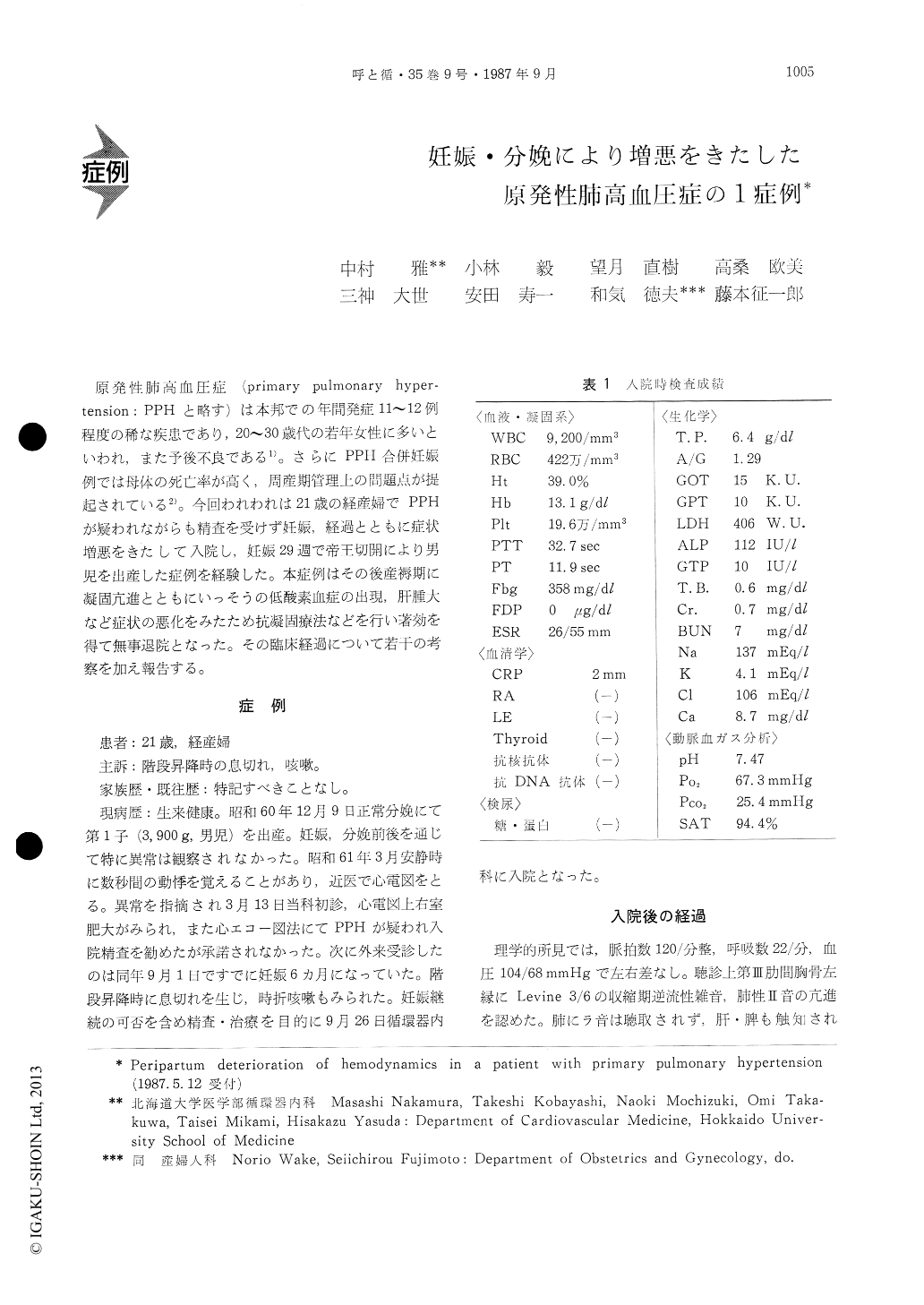
原発性肺高血圧症(primary pulmonary hyper—tension:PPHと略す)は本邦での年間発症11〜12例程度の稀な疾患であり,20〜30歳代の若年女性に多いといわれ,また予後不良である1)。さらにPPH合併妊娠例では母体の死亡率が高く,周産期管理上の問題点が提起されている2)。今回われわれは21歳の経産婦でPPHが疑われながらも精査を受けず妊娠,経過とともに症状増悪をきたして入院し,妊娠29週で帝王切開により男児を出産した症例を経験した。本症例はその後産褥期に凝固亢進とともにいっそうの低酸素血症の出現,肝腫大など症状の悪化をみたため抗凝固療法などを行い著効を得て無事退院となった。その臨床経過について若干の考察を加え報告する。
A 21-year-old woman was admitted to Hokkaido University Hospital during the 24 th week of her second pregnancy complaining of dyspnea on exert-ion. Prior to this event she had been well and her previous pregnancy was uneventful. Her heart rate was 116 bpm, BP, 104/68 mmHg, and respirations, 22/ min. There was an accentuated P2 and 3/6 systolic murmur. Electrocardiogram showed right axis devi-ation and right ventricular hypertrophy. Chest roe-ntrogram showed prominence of the main pulmonary arteries with cardiomegaly. Arterial PO2, was 67 mm-Hg in room air. Arterial PO2 increased to 96 mmHg with oxygen (nasal 2l/min). In the 25th week of gestagen, cardiac catheterization was performed. It confirmed pulmonary hypertension (75/40 mmHg) and no shunts were detected by oximetric studies. To promote fetal maturity Dexamethasone was ad-ministered.
By the 29 th week, dyspnea, cough and chest pain became more prominent. Arterial PO2 decreased to 78 mmHg in spite of oxygen administration and platelet aggregation level was abnormally elevated. Because of progressive symptoms, we decided to perform cae-sarian section. A Swan-Ganz catheter was placed in the PA, the pressure was 68/34 mmHg and epidural anesthesia with Xylocaine was employed.
Two minutes after delivery, BP and PA pressure suddenly decreased and she became unconscious. But she recovered in a few minutes by administration of pure oxygen, Dobutamine and Nitroglycerin.
On the next morning of delively, PA pressure was 50/25 mmHg, HR was 100 bpm and her symptoms diminished. But after delivery fibrinogen and platelet aggregation levels were abnormally elevated.
On the 7 th day, she complained of dyspnea again and became cyanotic. Arterial PO2 was 63 mmHg with oxygen administered by mask (FIO2 50%). Onthe 12 th day, cardiac catherization was repeated and PA pressure was 84/45 mmHg. HR also in-creased to 120 bpm. Trial of vaso-dilator therapy with Diltiazem, Captopril or Hydraladine was not effective. Following administration of Heparin, anti-coagulation therapy with Warfarin was started. Platelet-inhibiting drug, Ticlopidine was added. These therapy caused symptomatic improvement. Fibrinogen and platelet aggregation levels decreasedto within normal limits. ISDN, which could reduce the PA pressure, was also added. She was discharged from hospital without oxygen administration 2 months after delivery.
This case suggests impared coagulation ability may cause the deterioration of primary pulmonary hypertension during peripartum. It may be related to pulmonary microemboli. Anti-coagulation therapy is effective to such a patient.
Copyright © 1987, Igaku-Shoin Ltd. All rights reserved.


