Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
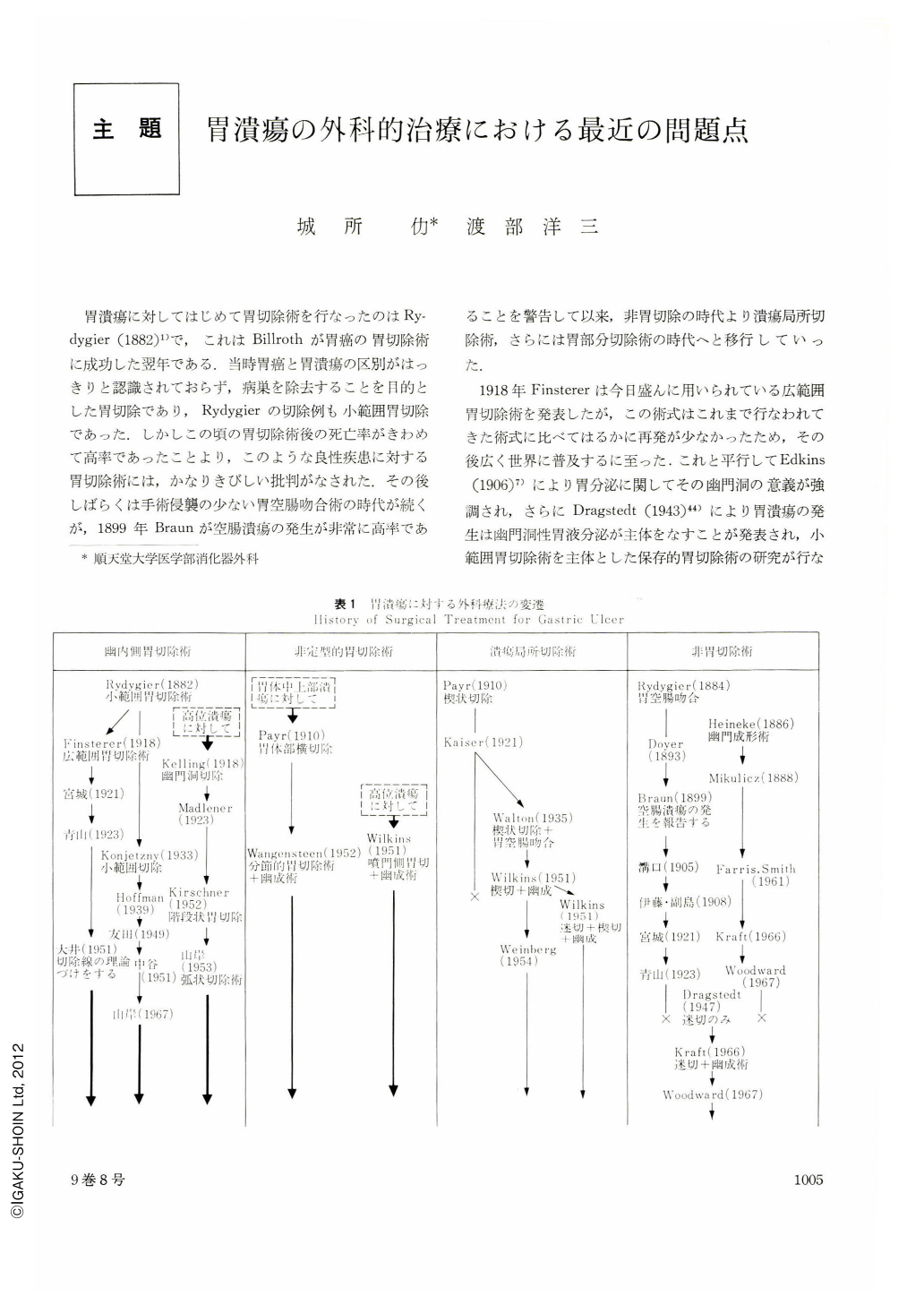
胃潰瘍に対してはじめて胃切除術を行なったのはRydygier(1882)1)で,これはBillrothが胃癌の胃切除術に成功した翌年である.当時胃癌と胃潰瘍の区別がはっきりと認識されておらず,病巣を除去することを目的とした胃切除であり,Rydygierの切除例も小範囲胃切除であった.しかしこの頃の胃切除術後の死亡率がきわめて高率であったことより,このような良性疾患に対する胃切除術には,かなりきびしい批判がなされた.その後しばらくは手術侵襲の少ない胃空腸吻合術の時代が続くが,1899年Braunが空腸潰瘍の発生が非常に高率であることを警告して以来,非胃切除の時代より潰瘍局所切除術,さらには胃部分切除術の時代へと移行していった.
1918年Finstererは今日盛んに用いられている広範囲胃切除術を発表したが,この術式はこれまで行なわれてきた術式に比べてはるかに再発が少なかったため,その後広く世界に普及するに至った.これと平行してEdkins(1906)7)により胃分泌に関してその幽門洞の意義が強調され,さらにDragstedt(1943)44)により胃潰瘍の発生は幽門洞性胃液分泌が主体をなすことが発表され,小範囲胃切除術を主体とした保存的胃切除術の研究が行なわれてきた.胃潰瘍の特殊型である高位潰瘍に対する術式は,Payr(1910)2)の楔状切除術,Kelling(1918)9)およびMadlener(1923)10)の幽門洞切除術をへて,Wilkins4)の噴門側胃切除術へと発展していった.
In Japan, a distal two-thirds resection of the stomach has been widely performed as an operative procedure for gastric ulcer. Recurrence of ulcer is notably rare following this surgical treatment but some problems do exist with it ; i. e., the patient treated regains scarcely in weight and his food intake is hardly restored to the preoperative level. More desirable, therefore, would be to select a surgical procedure which permits preservation of a greater part of the stomach without incurring the risk of recurrence.
The maximum acid output that can be tolerated by the duodenal and jejunal mucosa is approximately 10 mEq/hr. and, when the acid secretion from the stomach exceeds this level, the intestinal mucosa may no longer tolerate the increased acidity and eventually ulceration develops. The mucosa lining the gastric wall, if it is normal, is more resistant to hydrochloric acid than the duodenal and jejunal mucosa, whereas in advanced cases of atrophic gastritis, ulceration may develop even in the presence of hypochlorhydria. The frequent site for development of atrophic gastritis is the pyloric region. Consequently, intensive surgical treatment for reduction of gastric acid secretion is mandatory in case which more or less pyloric mucosa is left on the remaining portion of stomach after gastrectomy. While no such operative measure would be necessary in a patient whose residual stomach is completely devoid of pyloric mucosa.
Antrectomy is indicated for gastric ulcer in areas below the angulus, as reduction of acid secretion by 80% or more can usually be attained by this procedure. Concomitant vagotomy is unnecessary.
Segmental gastric resection or proximal gastric resection may be the choice of surgical treatment for ulcers situated either in the supraangular portion or in the more upper portion of stomach. As the pylorus is left intact by these operations, it is highly advisable to resect the stomach extensively insomuch as 80 to 90% of the gastric fundus.
Juxtapyloric ulcer and gastroduodenal ulcers are the only conditions requiring vagotomy for the treatment of gastric ulcer.
Copyright © 1974, Igaku-Shoin Ltd. All rights reserved.


