Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- サイト内被引用 Cited by
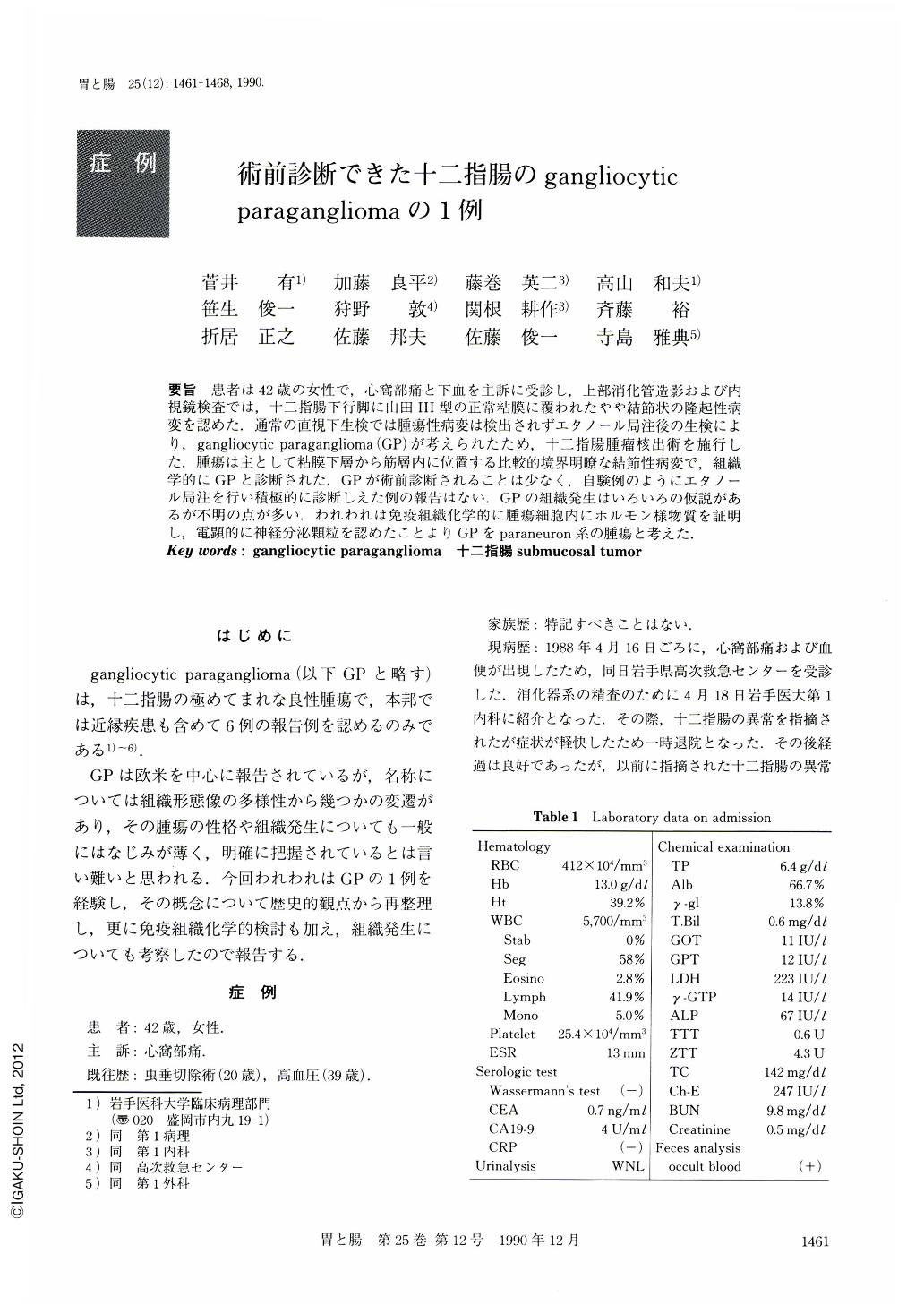
要旨 患者は42歳の女性で,心窩部痛と下血を主訴に受診し,上部消化管造影および内視鏡検査では,十二指腸下行脚に山田Ⅲ型の正常粘膜に覆われたやや結節状の隆起性病変を認めた.通常の直視下生検では腫瘍性病変は検出されずエタノール局注後の生検により,gangliocytic paraganglioma(GP)が考えられたため,十二指腸腫瘤核出術を施行した.腫瘍は主として粘膜下層から筋層内に位置する比較的境界明瞭な結節性病変で,組織学的にGPと診断された.GPが術前診断されることは少なく,自験例のようにエタノール局注を行い積極的に診断しえた例の報告はない.GPの組織発生はいろいろの仮説があるが不明の点が多い.われわれは免疫組織化学的に腫瘍細胞内にホルモン様物質を証明し,電顕的に神経分泌顆粒を認めたことよりGPをparaneuron系の腫瘍と考えた.
A 42-year-old woman was admitted to the hospital of Iwate Medical University with epigastralgia and gastrointestinal bleeding as her chief complaints.
An upper gastrointestinal series and endoscopic examination revealed a polypoid tumor in the second portion of the duodenum. Biopsy specimens obtained from this polyp were histologically normal. Using topical injection of pure ethanol as our method, we succeeded in obtaining some tumor tissue. At operation, a discrete 1.5 cm mass was removed from the duodenum.
The tumor was located in the submucosa and muscularis of the duodenum. There was no capsule, but the lesion was well circumscribed. Histologically, the tumor was composed of 1) polygonal or columnar epithelioid cells, 2) mature ganglion cells, 3) spindle cells arranged in broad fascicles. A “zellballen” pattern was also seen. Grimelius stains were negative.
Electron-microscopic examination of the epithelioid tumor cells showed numerous secretory granules, which were of moderate density and measured 100-300 nm.
The results of immunohistochemical studies were as follows: The epithelioid cells stained strongly with neuron-specific enolase (NSE), somatostatin, pancreatic polypeptide, cytokeratin; ganglion cells stained with NSE; spindle cells were positive for S-100 protein. There was no cellular atypism or mitosis to suggest malignancy. The diagnosis was gangliocytic paraganglioma (GP).
Although the histogenesis of duodenal GP remains unclear, many theories have been postulated. It has been suggested that the tumor arises from embryonic celiac ganglion, from stem cells of intestinal mucosa, from Meissner's plexus, or from the pancreas. The latest hypothesis proposes that duodenal GP is a hyperplastic or neoplastic proliferation of endodermallyderived epithelial cells originating from the ventral primordium of the pancreas, neuroectodermal ganglion cells and spindle cells. This hypothesis conflicts with the fact that paraganglia are of neuroectodermal origin. We propose that it is a neoplastic lesion arising from the paraneuron family.
Copyright © 1990, Igaku-Shoin Ltd. All rights reserved.


