Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
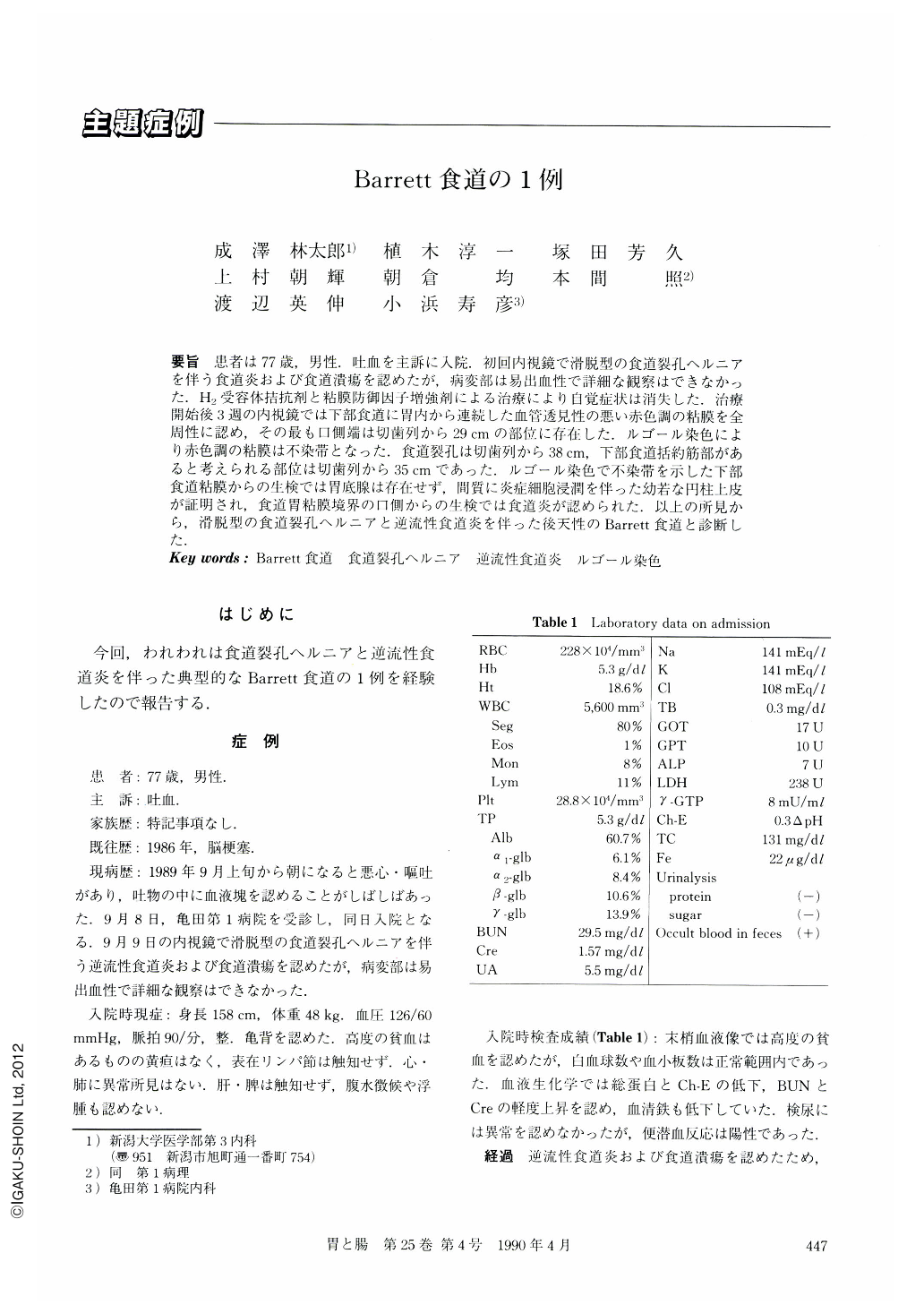
要旨 患者は77歳,男性.吐血を主訴に入院.初回内視鏡で滑脱型の食道裂孔ヘルニアを伴う食道炎および食道潰瘍を認めたが,病変部は易出血性で詳細な観察はできなかった.H2受容体拮抗剤と粘膜防御因子増強剤による治療により自覚症状は消失した.治療開始後3週の内視鏡では下部食道に胃内から連続した血管透見性の悪い赤色調の粘膜を全周性に認め,その最も口側端は切歯列から29cmの部位に存在した.ルゴール染色により赤色調の粘膜は不染帯となった.食道裂孔は切歯列から38cm,下部食道括約筋部があると考えられる部位は切歯列から35cmであった.ルゴール染色で不染帯を示した下部食道粘膜からの生検では胃底腺は存在せず,間質に炎症細胞浸潤を伴った幼若な円柱上皮が証明され,食道胃粘膜境界の口側からの生検では食道炎が認められた.以上の所見から,滑脱型の食道裂孔ヘルニアと逆流性食道炎を伴った後天性のBarrett食道と診断した.
A 77-year-old male was admitted to Kameda Daiichi hospital with a complaint of hematemesis.
Physical examination showed severe anemia and kyphosis. The first endoscopic examination revealed esophageal ulcer with sliding hiatus hernia and reflux esophagitis. Blood over the mucosa, however, prevented us from observing bleeding lesions in detail. He was treated with an H2-receptor antagonist and mucosal defensive agents, resulting in the disappearance of clinical symptom. The second endoscopic examination which was performed three weeks later showed an extensive reddish lesion not stained by Lugol's solution from the cardia. The lesion extended throughout the mucosa of the lower esophagus with the oral margin 29 cm distal to the dental arch. Biopsy specimens obtained from the lesion demonstrated regenerating columnar epithelia with goblet cell metaplasia but without fundic glands. Esophagogram revealed sliding hiatus hernia but failed to detect Barrett's esophagus.
Based on these findings, the patient was diagnosed as having typical case of acquired Barrett's esophagus with sliding hiatus hernia and reflux esophagitis.
Copyright © 1990, Igaku-Shoin Ltd. All rights reserved.


