Japanese
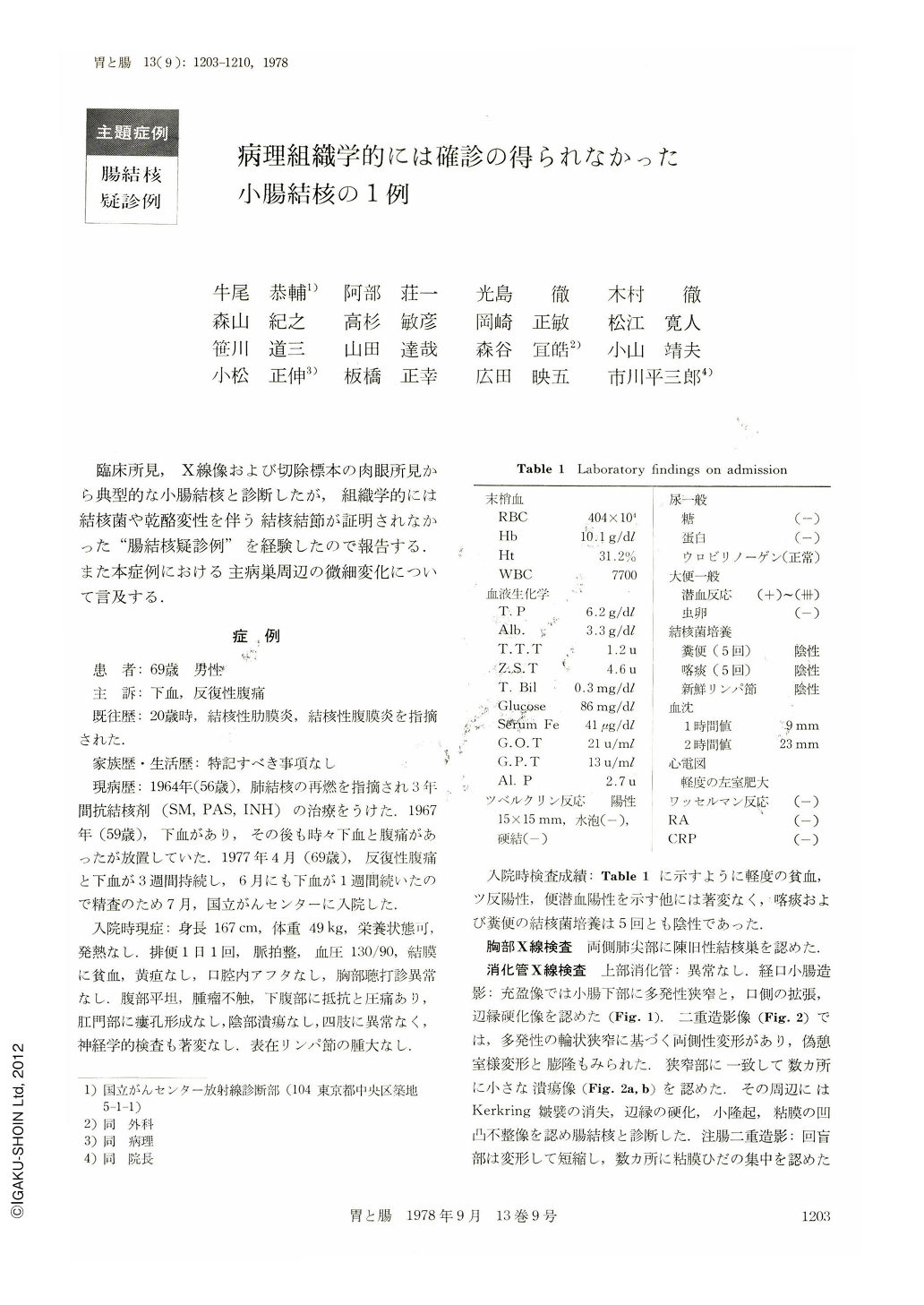
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- サイト内被引用 Cited by
臨床所見,X線像および切除標本の肉眼所見から典型的な小腸結核と診断したが,組織学的には結核菌や乾酪変性を伴う結核結節が証明されなかった“腸結核疑診例”を経験したので報告する.また本症例における主病巣周辺の微細変化について言及する.
症 例
患 者:69歳 男性
主 訴:下血,反復性腹痛
既往歴:20歳時,結核性肋膜炎,結核性腹膜炎を指摘された.
家族歴・生活歴:特記すべき事項なし
現病歴:1964年(56歳),肺結核の再燃を指摘され3年間抗結核剤(SM,PAS,INH)の治療をうけた.1967年(59歳),下血があり,その後も時々下血と腹痛があったが放置していた.1977年4月(69歳),反復性腹痛と下血が3週間持続し,6月にも下血が1週間続いたので精査のため7月,国立がんセンターに入院した.
We describe here a 69 years old man complaining of melena and recurrent abdominal pain. At the age of 20 he had been afflicted with tuberculous pleuritis and peritonitis.
Thirteen years before at the age of 56 he had been treated with antituberculosis agents (SM, PAS and INH) because of the relapse of lung tuberculosis. Since April 1977 melena and abdominal pain frequently occurred, so that he was admitted to the National Cancer Center Hospital for complete checkup. His general condition was good. Objectively only slight resistence and tenderness were noticed in the lower abdomen. Laboratory examination showed positive Mantoux reaction and slight anemia. The stools were continuously positive for occult blood. Culture of the sputum and feces for tubercle bacillus was negative.
X-ray picture of the chest showed bilaterally old apical tuberculous lesions. In the barium meal study the upper digestive tract was normal, but double contrast study of the small intestine showed stenoses at six places in the ileum. Here were found linear ulcers and their scars running perpendicular to the longitudinal axis of the intestine. They were surrounded with areas of scar and atrophic mucosa. A diagnosis of intestinal tuberculosis was then made. Surgical intervention revealed no adhesion between the peritoneum and mesentery, and there was hardly found any fistule or lymph-node swelling. The resected ileum, 40cm long including the stenosed segments, showed multiple linear ulcers surrounded by “the atrophic areas accompanied with ulcer scars.”T ubercle bacillus was negative from the culture of the fresh lymph nodes. Bacteriologic and histologic examinations of the resected specimen revealed no caseating granuloma.
Multiple occurrence of ulcers and their scars was also recognized.
Only a single atrophic non-caseating granuloma was finally detected in the submucosa of the atrophic area. Histologically, the present case was seemed probable intestinal tuberculosis.
Clinically, however, especially in the macroscopic findings of the resected specimen and X-ray study, the diagnosis was most likely intestinal tuberculosis. Finally and collectively, we believe this case was intestinal tuberculosis.
Copyright © 1978, Igaku-Shoin Ltd. All rights reserved.


