Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- サイト内被引用 Cited by
胃の内面を裏打ちしている粘膜は幽門腺粘膜・胃底腺粘膜・噴門腺粘膜と呼ばれていて,それらは胃に固有な粘膜である.一方,それら粘膜は腸の上皮に類似したL皮によって置き換えられる場合があり,それを腸上皮化生と呼んでいる.このように,胃の粘膜は本質的に胃固有粘膜と腸上皮化生粘膜との2つに大別することができる.
ひるがえって,筆者らは胃癌の組織発生に関し「未分化型癌は胃固有粘膜から,一方,分化型癌は胃の腸上皮化生粘膜から発生し,癌発生後は,癌もまた正常細胞の分化の過程を模倣している」とのことを主張している1)2).この組織発生からは,「胃固有粘膜の一つである胃底腺粘膜から発生する癌の組織型は,未分化型癌であらねばならぬ」という命題が派生する.なぜならば,胃癌の好発部位は幽門前庭部で,胃癌組織発生の概念を導くにあたっては対象の大部分が幽門前庭部に発生した癌であり,幽門前庭部は一般的に幽門腺粘膜で裏打ちされている場であるからである.この命題を証明するための必要かつ十分条件は,胃切除時点で癌が腸上皮化生のない胃底腺粘膜領域に存在していてその組織型が未分化型であり,そして,腸上皮化生のない胃底腺粘膜領域を限界づける境界が時間の経過とともに不可逆的にその領域の収縮する方向に変化するか,あるいはその境界が不変であることである.なぜならば,胃切除時点で癌が腸上皮化生のない胃底腺粘膜領域に存在していても,その領域を限界づける境界線が経時的に可逆的に変化するものであるならば,その癌が発生した時点では腸上皮化生をともなう胃底腺粘膜領域であったかもしれないからである.以上のようなことから,腸上皮化生のない胃底腺粘膜領域を限界づける線をF境界線(F boundary line)と定義して,その経時的変化を報告している3).
A boundary is formed where two mucosae of a different nature contact in the stomach. The boundary formed between the pyloric and fundic gland mucosae is generally called the “Intermediate zone”, and is defined as an area where the parietal cells or chief cells appear. This definition is based on a cellular level. However, it becomes difficult to grasp the general tendency of pattern of the intermediate zone, because the boundary formed at the histological level, is defined at the cellular level and the parietal cells are sometimes present at the pyloric glands located in the antrum. Furthermore, the definition does not consider metaplastic epithelium of intestinal type which is associated with a certain lesions of the stomach. The definition is only anatomical. From the clinicopathological view-point, it is necessary to consider intestinal metaplasia in definition of a boundary.
This paper is to study change with increasing age of the boundary line defined clinico-pathologically and its clinico-pathological significances. Object consists of 756 stomachs resected for small carcinoma or benign lesion. Those stomachs were examined histologically by means of serial cutting method as shown in Figs. 8a~8e.
Intestinal metaplasia first occurs in the pyloric gland mucosa and gradually spreads over the entire mucosa of the stomach. The boundary line can be defined as the follows: (1) F boundary line is the margin of the fundic gland mucosa without intestinal metaplasia, and (2) f boundary line is the margin of area in which the fundic gland mucosa is focally together with intestinal metaplasia (Fig. 6). The area encircled by these two lines is called “Intermediate area of metaplastic fundic gland mucosa”.
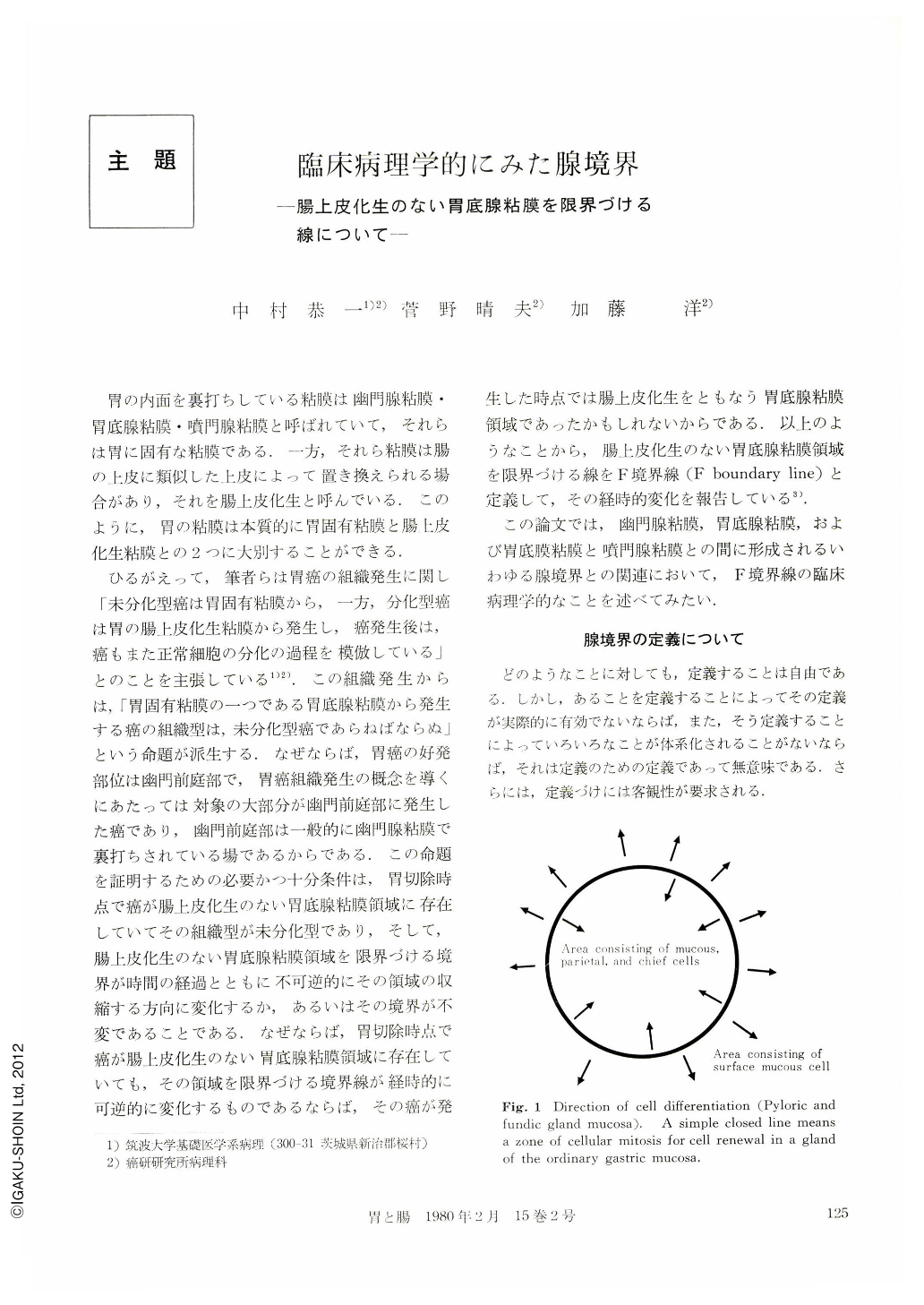
Morphologically, there is a variety of the F boundary line patterns, but the F boundary lines are divided essentially into two patterns, Ordinary pattern (Figs. 8a, b) and Atrophic pattern (Figs. 8c, d, e). The ordinary pattern has the two F boundary lines. One is formed between the pyloric gland and the funclic gland mucosae (Fig. 8a), or between the fundic gland mucosa with intestinal metaplasia and the fundic gland mucosa without intestinal metaplasia (Fig. 8b), and the other between the latter fundic gland mucosa and the cardiac gland mucosa (Fig. 8a). These boundary lines encircle the lumen of the stomach on the wall (Fig. 9). In other words, the curved surface of the fundic gland mucosa without intestinal metaplasia is a girdle encircling the lumen of the stomach. The F boundary line of the atrophic pattern is only one in number, and is a simple closed curve which appears around the corpus through the greater curvature (Fig. 8c, d). In other words, the area of the fundic gland mucosa without intestinal metaplasia is a curved surface encircled by the F boundary line on the stomach wall (Fig. 9).
The distance between the pyloric ring and the Fboundary line of the ordinary pattern widely varies in each case. The area of the fundic gland mucosa encircled by F boundary line of the atrophic pattern widely varies in each case. Its limit is a state in which the F boundary line is reduced to a point. In other words, it is a state in which the F boundary line disappears and only the f boundary line exists. The ratio of the ordinary pattern to the atrophic pattern decreases with age (Table 1 and Fig. 10). In other words, with increasing age, the ordinary pattern decreases, and the atrophic pattern increases. It is concluded from the data obtained and those findings mentioned above that the two F boundary lines become closer to each other, as age increases, and the simple closed curve which is formed as the result of fusion of both F boundary lines on the lesser curvature is reduced to a point (Fig. 11). The shifting of the F boundary line is generally irreversible. This means that the area of the fundic gland mucosa becomes reduced with age.
As to grades of intestinal metaplasia, tendency of the ratio of non-to mild-intestinalization to moderateto marked-intestinalization by age group is almost the same as that of the F boundary line (Table 2, Fig. 12). Statistically, there is a relationship between the degree of intestinalization and the pattern of the F boundary line (Table 3). In other words, the mucosa which are markedly intestinalized belong to the atrophic pattern and those whose intestinalization is less marked belong to the ordinary pattern in most instances. The shifting of the F boundary line can phenomenally be recognized as atrophy with disappearance of the fundic gland mucosa or replacement of the latter by the intestinalized fundic gland mucosa.
As to the pattern of the F boundaly line and intestinalization by sex and age, it is seen that the ratio of the ordinary pattern to the atrophic pattern, and the ratio of non-to mild-intestinalization to moderateto marked-intestinalization generally become 1 in men between 30 and 40 years of age, and in women between 49 and 50 years of age (Figs. 13 and 14). The atrophic pattern and grade of intestinalization appear and become marked at an earlier age in men than in women.
It is clear that the carcinoma situated in the interior area of the F boundary line arose from the fundic gland mucosa, regardless of its size, because the interior encircled by the F boundary line consists of the fundic gland rnucosa without intestinal metaplasia, and shifting of the F boundary line is irreversible with increasing age. The histological type of all carcinoma that has been histologically demonstrated to be completely limited to the interior encircled by the F boundary line, is of undifferentiated type (diffuse carcinoma) regardless of the size of the carcinoma (Table 5). This result clearly demonstrates that the undifferentiated carcinoma arises from the fundic gland mucosa, that is to say from the ordinary mucosa. This evidence decisively demonstrates one of the hypothesis, that the undifferentiated carcinoma arises from the ordinary mucosa.
The area of the fundic gland mucosa macroscopically almost corresponds to that of marked Inucosal fold. The histological pattern of cancer which has developed in the fundic gland mucosa area is of the undifferentiated type. The undifferentiated carcinoma is apt to become ulcerative. Therefore, the cancer in the fundic gland mucosa spatially overlaps an ulcerative lesion in most instances (Table 6). Whereas, a benign ulcer develops quite rarely in the fundic gland mucosa area (Table 4). Accordingly, it is rare that we are mistaken in making a diagnosis of cancer of the undifferentiated type, when roentgenological and/or endoscopic examinations reveal an ulcerative lesion entirely encircled by remarkable rnucosal fold, even if no finding of cancer is obtained.
Copyright © 1980, Igaku-Shoin Ltd. All rights reserved.


