Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
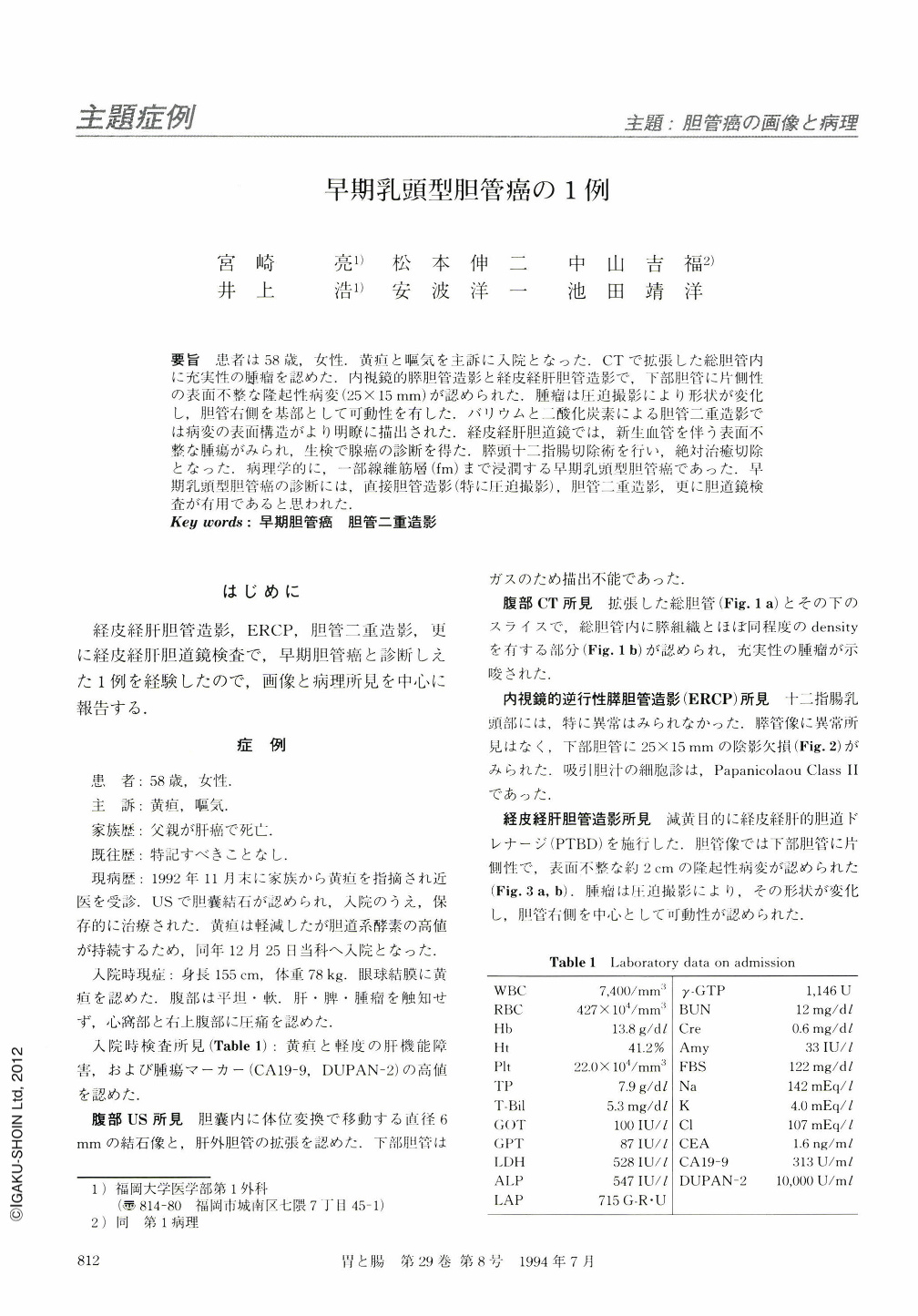
要旨 患者は58歳,女性.黄疸と嘔気を主訴に入院となった.CTで拡張した総胆管内に充実性の腫瘤を認めた.内視鏡的膵胆管造影と経皮経肝胆管造影で,下部胆管に片側性の表面不整な隆起性病変(25×15mm)が認められた.腫瘤は圧迫撮影により形状が変化し,胆管右側を基部として可動性を有した.バリウムと二酸化炭素による胆管二重造影では病変の表面構造がより明瞭に描出された.経皮経肝胆道鏡では,新生血管を伴う表面不整な腫瘍がみられ,生検で腺癌の診断を得た.膵頭十二指腸切除術を行い,絶対治癒切除となった.病理学的に,一部線維筋層(fm)まで浸潤する早期乳頭型胆管癌であった.早期乳頭型胆管癌の診断には,直接胆管造影(特に圧迫撮影),胆管二重造影,更に胆道鏡検査が有用であると思われた.
A 58-year-old female was admitted to our hospital because of jaundice. CT disclosed a high density ovoid mass in the distal portion of the dilated common duct, adjacent to the duodenal papilla. Endoscopic retrograde cholangiography revealed a tumor as a filling defect. Double contrast study through the percutaneous transhepatic biliary drainage (PTBD) further characterized the tumor as being papillary in nature. The cholangioscopy via the PTBD visualized the tumor with a granular surface and the diagnosis of the biopsied specimen was adenocarcinoma. Pancreatoduodenectomy was performed. The histological examination of the resected specimen revealed that the tumor was 47X2OX18mm in size, and the invasion of cancer cells was limited to within the fibromuscular layer of the common duct. The present study demonstrates that a cholangiogram with double contrast study and cholangioscopy are of significance in making diagnosis of early bile duct cancer.
Copyright © 1994, Igaku-Shoin Ltd. All rights reserved.


