Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
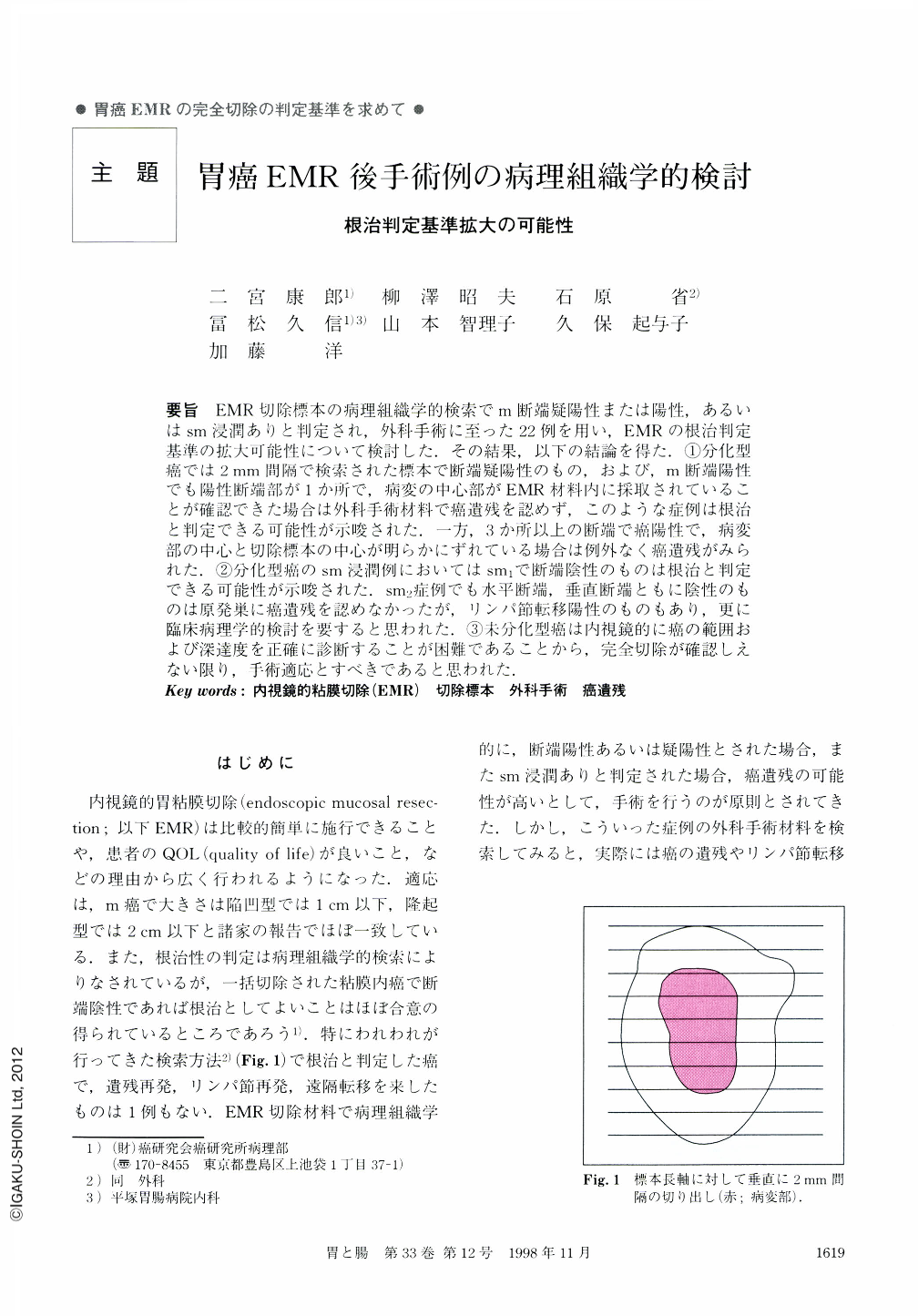
要旨 EMR切除標本の病理組織学的検索でm断端疑陽性または陽性,あるいはsm浸潤ありと判定され,外科手術に至った22例を用い,EMRの根治判定基準の拡大可能性について検討した.その結果,以下の結論を得た.①分化型癌では2mm間隔で検索された標本で断端疑陽性のもの,および,m断端陽性でも陽性断端部が1か所で,病変の中心部がEMR材料内に採取されていることが確認できた場合は外科手術材料で癌遺残を認めず,このような症例は根治と判定できる可能性が示唆された.一方,3か所以上の断端で癌陽性で,病変部の中心と切除標本の中心が明らかにずれている場合は例外なく癌遺残がみられた.②分化型癌のsm浸潤例においてはsm1で断端陰性のものは根治と判定できる可能性が示唆された.sm2症例でも水平断端,垂直断端ともに陰性のものは原発巣に癌遺残を認めなかったが,リンパ節転移陽性のものもあり,更に臨床病理学的検討を要すると思われた.③末分化型癌は内視鏡的に癌の範囲および深達度を正確に診断することが困難であることから,完全切除が確認しえない限り,手術適応とすべきであると思われた.
In order to examine the possibility of broadening the histological criteria for diagnosing as cured patients who have undergone endoscopic mucosal resection (EMR), we studied 22 cases subjected to surgery after EMR due to cancer-positive cut margin (s) in the mucosa, cancer positive end cuts from the resected material, or submucosal, or submucosal invasion (sm). All histological examinations were performed on EMR materials sectioned at 2 mm-intervals.
Criteria for Classification as Cured.
For differentiated mucosal gastric cancer treated by EMR, the center of the lesion must be captured with only one cancer-positive cut-end in the EMR material (all cases of this type in the present study had at least one positive cut end). The 2 cases which met these criteria had no residual cancer in their operated material. When the lesion apparently extended the EMR material with more than 2 cancer-positive cut ends, residua cancer was observed without exception in the operated material (there were no cases of exactly 2 cancer positive cut-ends).
For differentiated type adenocarcinomas with sm-invasion, predictive criteria for curability and the avoidance of lymph node metastases include sm-invasion limited to 200~300 μm from the mucosal muscle (sml) without any cancer-positive cut ends.
However, when it comes to undifferentiated type adenocarcinomas, all patients subjected to surgery after EMR had residual cancer in the operated materials. One patient appeared macroscopically to have been cured by EMR, but, histologically, cancer-positive cut ends were observed in the EMR material. In general, it is difficult macroscopically determine the areas and invasion-depths of undifferentiated type adenocarcinomas. Accordingly, unless complete resection is assured, cases with undifferentiated type adenocarcinomas should always be followed by additional surgery.
For differentiated type adenocarcinomas with and without sm-invasion, the current study suggests the possibility of broadening histological criteria for diagnosing as cured patients who have undergone EMR. For undifferentiated type adenocarcinomas, this possibility is not indicated.
Copyright © 1998, Igaku-Shoin Ltd. All rights reserved.


