Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- サイト内被引用 Cited by
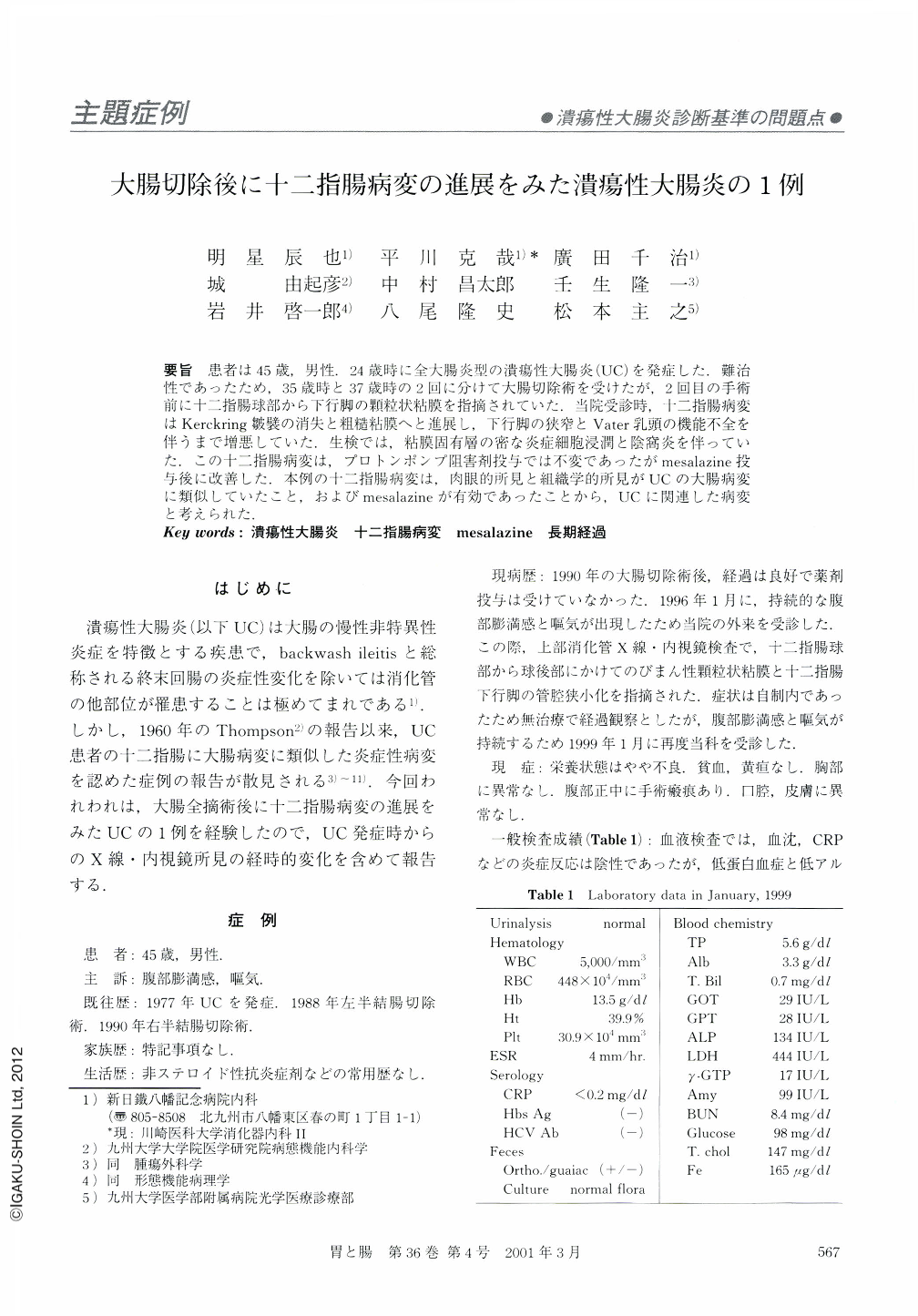
要旨 患者は45歳,男性.24歳時に全大腸炎型の潰瘍性大腸炎(UC)を発症した.難治性であったため,35歳時と37歳時の2回に分けて大腸切除術を受けたが,2回目の手術前に十二指腸球部から下行脚の顆粒状粘膜を指摘されていた.当院受診時,十二指腸病変はKerckring皺襞の消失と粗糙粘膜へと進展し,下行脚の狭窄とVater乳頭の機能不全を伴うまで増悪していた.生検では,粘膜固有層の密な炎症細胞浸潤と陰窩炎を伴っていた.この十二指腸病変は,プロトンポンプ阻害剤投与では不変であったがmesalazine投与後に改善した.本例の十二指腸病変は,肉眼的所見と組織学的所見がUCの大腸病変に類似していたこと,およびmesalazineが有効であったことから,UCに関連した病変と考えられた.
A 45-year-old male visited our hospital, because of continuing abdominal distension and nausea. He had a prior diagnosis of ulcerative colitis, which had been treated by total colectomy nine years previously. Duodenography and duodenoscopy revealed that he had a diffuse duodenal lesion accompanied by a stenosed area in the second portion of the duodenum. Histologically, the duodenal lesion had features comparable to those in ulcerative colitis. A retrospective analysis of the case suggested that his duodenal lesion had deteriorated after the colectomy, during which period no specific treatment had been applied. While the duodenitis did not respond to a proton-pump inhibitor, it improved obviously after the administration of mesalazine. Our case suggests that the duodenum is a possible site of involvement in ulcerative colitis, although such occurrence seems to be extremely rare.
Copyright © 2001, Igaku-Shoin Ltd. All rights reserved.


