Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
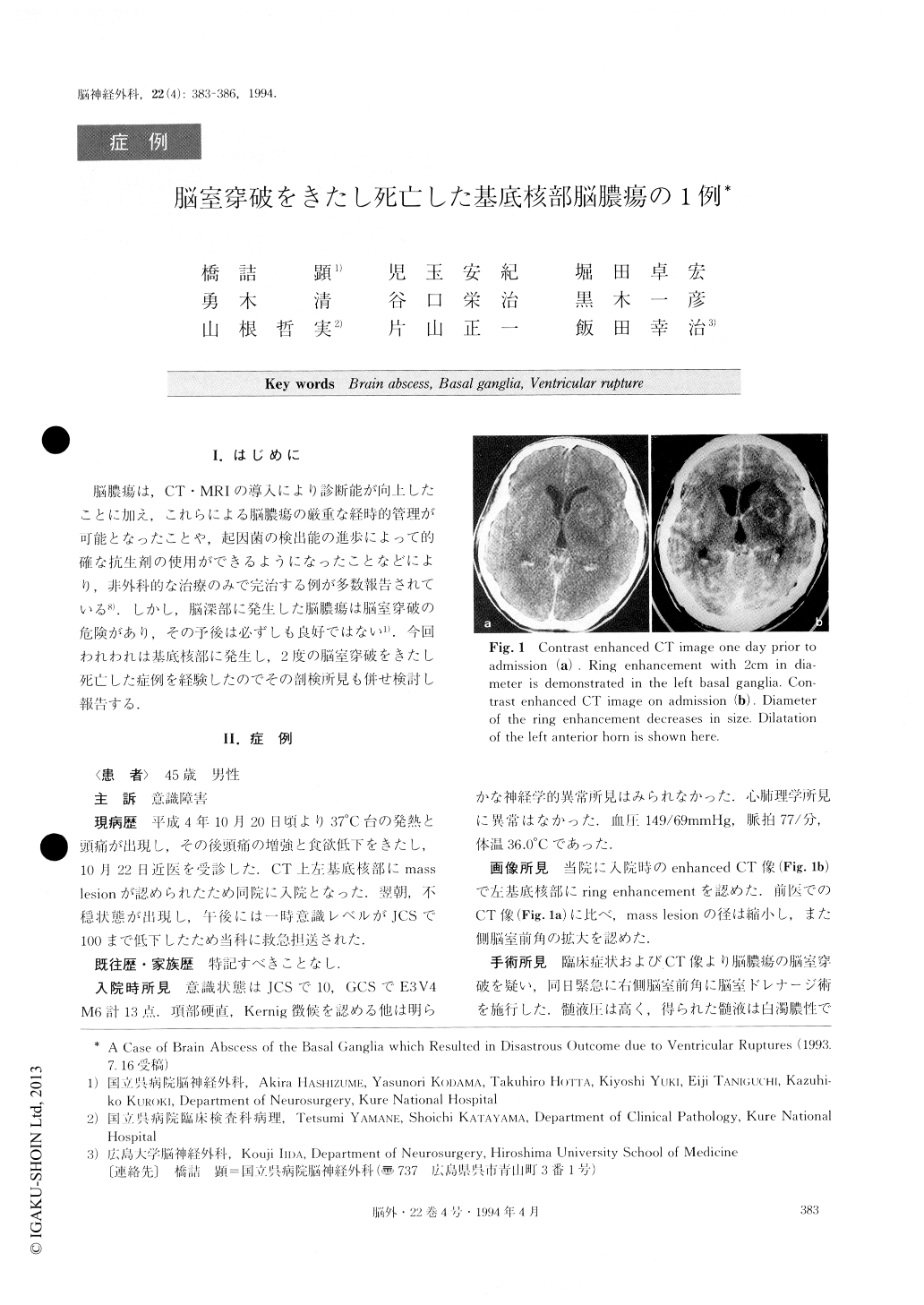
脳膿瘍は,CT・MRIの導入により診断能が向上したことに加え,これらによる脳膿瘍の厳重な経時的管理が可能となったことや,起因菌の検出能の進歩によって的確な抗生剤の使用ができるようになったことなどにより,非外科的な治療のみで完治する例が多数報告されている8).しかし,脳深部に発生した脳膿瘍は脳室穿破の危険があり,その予後は必ずしも良好ではない1).今回われわれは基底核部に発生し,2度の脳室穿破をきたし死亡した症例を経験したのでその剖検所見も併せ検討し報告する.
A case of deep-seated brain abscess that ruptured twice into the ventricle and resulted in death is pre-sented.
A 45-year-old man had experienced pyrexia and headache for 3 days before admission. On admission he was somnolent (GCS: 13) but there were no abnormal neurological findings except nuchal rigidity and Ker-nig's sign. Computed tomography (CT) scan showed a ring enhanced mass near the left caudate head and di-lated ventricles. In comparison with CT performed at the former hospital it was diagnosed that a rupture into the ventricle of the brain abscess had occurred. Ven-tricular drainage was performed at once and white purulent cerebrospinal fluid was obtained. Thereafter, he was treated with some antibiotics and his conditions seemed to stabilize for a while. Serial CT images de-monstrated that the size of the abscess seemed to be enlarging. Just when we planned to undertake stereotactic aspiration, the second ventricular rupture occurred and he died.
According to this case, it is suggested that once a deep-seated brain abscess near the ventricular system is suspected, it should be aspirated by means of CT-guided stereotactic surgery immediately.
Copyright © 1994, Igaku-Shoin Ltd. All rights reserved.


