Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
糖尿病と膵腫瘤
[症例1]
患者 63歳,男性.
主訴 なし.
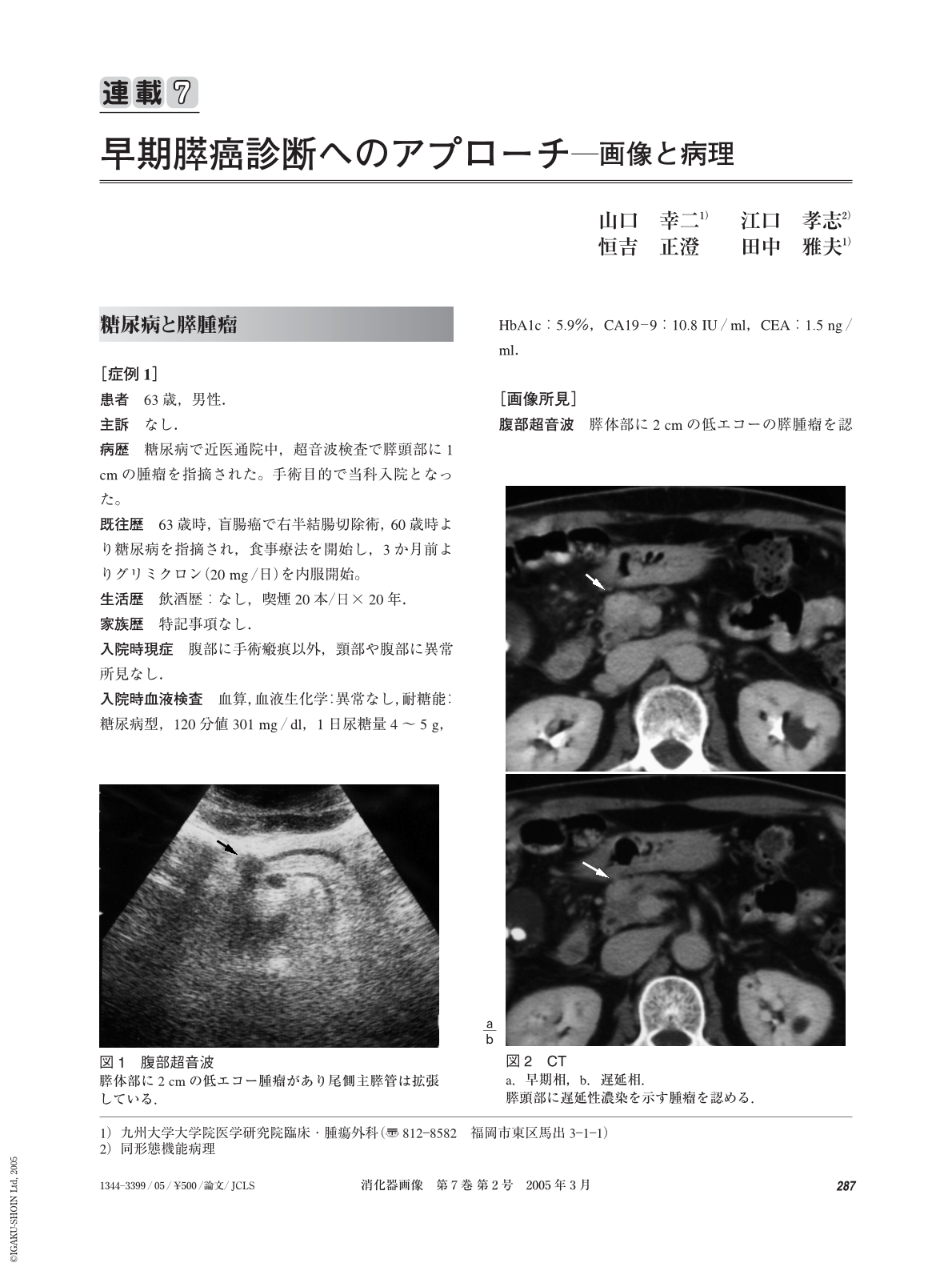
病歴 糖尿病で近医通院中,超音波検査で膵頭部に1 cmの腫瘤を指摘された。手術目的で当科入院となった。
既往歴 63歳時,盲腸癌で右半結腸切除術,60歳時より糖尿病を指摘され,食事療法を開始し,3か月前よりグリミクロン(20 mg/日)を内服開始。
生活歴 飲酒歴:なし,喫煙20本/日×20年.
家族歴 特記事項なし.
入院時現症 腹部に手術瘢痕以外,頸部や腹部に異常所見なし.
入院時血液検査 血算,血液生化学:異常なし,耐糖能:糖尿病型,120分値301 mg/dl,1日尿糖量4~5 g,HbA1c:5.9%,CA19-9:10.8 IU/ml,CEA:1.5 ng/ml.
Cace1
A 65-year-old man under the control of diabetes showed deterioration of diabetes and ultrasonography showed a pancreatic head mass, measuring 1.5 cm. Computed tomography and magnetic resonance imaging also showed a pancreatic head mass with delayed enhancement. Endoscopic retrograde pancreatography showed a stenosis of the main pancreatic duct and dilatation of the upper stream ducts. Brushing cytology of the stenosis of the main pancreatic duct showed atypical cells highly suggestive of malignancy. Pylorus preserving pancreatoduodenectomy with D2 lymph node dissection was performed under the diagnosis of pancreatic head cancer. Intraoperative radiation therapy(20 Gy)was also done. Histological examination showed a well differentiated adenocarcinoma, measuring 1.5 cm. Lymph node metastasis was not evident and surgical margins were free of cancer cells. After operation, radiation therapy was added and transarterial chemotherapy was performed. Arterial rupture from pseudoaneurysm occurred 2 years and 7 months after the operation and he unfortunately died of bleeding without signs of recurrence on imagings.
Case2
A 62-year-old man was diagnosed as having diabetes mellitus and hepatocellular carcinoma on liver cirrhosis five years ago. Ethanol injection therapy was performed for hepatocellular carcinoma. During follow-up ultrasonography detected a pancreatic body mass, measuring 1.5 cm. Serum level of CA19―9 was elevated to 359.9 IU/ml and CEA within normal limits. Computed tomography and magnetic resonance imaging also showed a pancreatic tail mass with delayed enhancement. Endoscopic retrograde pancreatography showed a complete obstruction of the main pancreatic duct and dilatation of the upper stream ducts. Distal pancreatectomy and splenectomy with D2 lymph node dissection was performed under the tentative diagnosis of pancreatic body cancer. Histological examination showed a well differentiated adenocarcinoma, measuring 1.5 cm. Lymph node metastasis was evident in the level 1 lymph node. After operation, uncontrollable ascites occurred. He was alive six months after operation and lost at the follow-up thereafter.
(Shokakigazo 2005 ; 2 : 287―294)
Copyright © 2005, Igaku-Shoin Ltd. All rights reserved.


