Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
多発性根神経炎(polyradiculoneuritis)にみられた網膜病変の1例を経験した.無菌性髄膜炎後に発症したもので,両眼黄斑部に出血と白斑が存在し,螢光眼底造影で,毛細血管の拡張,透過性亢進,毛細血管瘤,細動脈の閉塞による無血管野などがみられ,ウイルス性網膜炎と診断した.起因ウイルスはパラインフルエンザ3型が疑われたが,断定はできなかった.
ウイルス性網膜炎と多発性根神経炎の合併症例の報告は現在までみられていないが,この両者はウイルス感染が引き金となったアレルギー反応という同一の発症機序が考えられるので,今後もさらに注意が必要であることを述べた.
A 46-year-old male developed acute aseptic meningitis, followed by bilateral decreasing vision and diplopia one week later. He was referred to us 3 weeks after manifestation of ocular signs.
The visual acuity was 0.6 in the right eye and 0.1 in the left. Retinal hemorrhages were disseminated in both eyes. Soft exudates were also seen in the macular area. Fluorescein angiography showed numerous capillary microaneurysms, patchy areas of capillary nonperfusion and increased permeabil-ity of retinal capillaries.
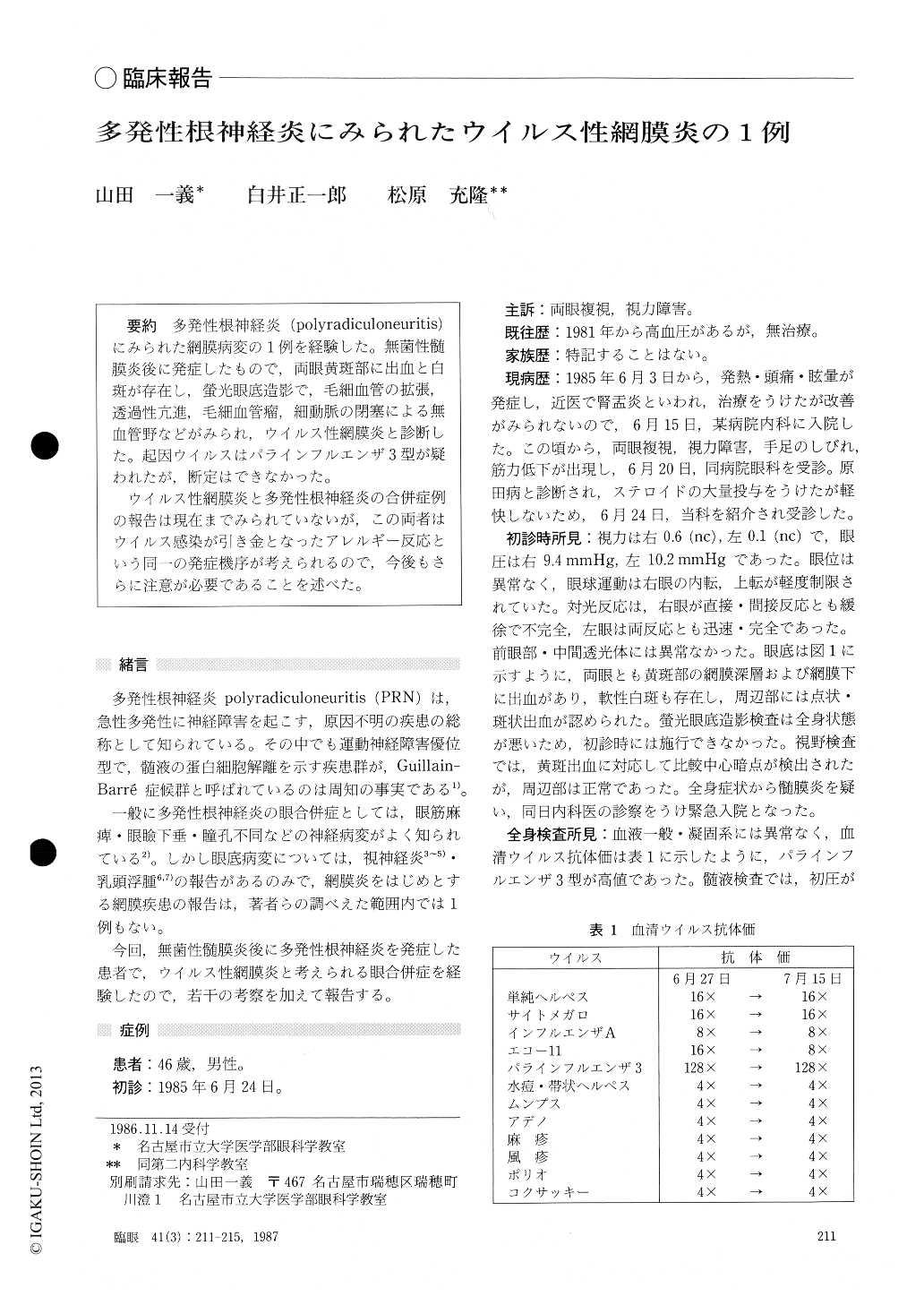
The titer for parainfluenza type 3 virus antibodywas 128x. Those for other viruses were normal.
Retinal hemorrhages and exudates were gradu-ally absorbed along with improvements in general condition of the patient. One year after onset of the disease, his visual acuity had improved to 1.2 in the right eye and 0.8 in the left.
He was diagnosed as presumed viral retinitis. It could not be determined whether the retinitis and polyradiculoneuritis were caused by the parain-fluenza virus as the common etiological factor. While there are scant reported cases of viral retinitis associated with polyradiculoneuritis, it is likely that both are consequences of hypersensitive reaction to a viral infection.
Rinsho Ganka (Jpn J Clin Ophthalmol) 41(3) : 211-215, 1987
Copyright © 1987, Igaku-Shoin Ltd. All rights reserved.


