Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
抄録 頭蓋内病変に伴う呼吸機能低下こおける神経性因子の関与の有無を明らかにするため,頭部外傷15例,脳血管障害4例,心停止蘇生後1例,計20例で,頭蓋内圧(ICP)が呼吸機能(肺シャント率,respiratoryindex,oxygenation index),肺血管外水分量,および循環動態(心係数,平均動脈圧,平均肺動脈圧,肺動脈楔入圧,全身血管抵抗,肺血管抵抗)に及ぼす影響を調べた。10例に誤嚥,肺炎,四肢の骨折を認めたため,これら10例を除いた10例を肺合併症除外群としてさらに検討した。全症例群ではICP⊥昇に伴って呼吸機能が低下する傾向を示したが,肺合併症除外群ではICPと呼吸機能低下との間に相関を認めなかった。肺血管外水分量もICPと特別の関係を示さなかった。循環動態の変化は,全症例群,肺合併症除外群ともICPと相関を示さなかった。しかし,肺合併症除外群において肺シャント率は10例中9例で10%以上の値を示した。その原因としては,DIC,sepsis,shock,大量の輸血等の全身合併症による影響が強く示唆されたことから,lCP亢進による神経原性肺水腫はは臨床的には非常に稀な病態であろうと考えられる。
Respiratory insufficiency following acutely ele-vated intracranial pressure (ICP) may occur as a result of pulmonary edema which is supposed to be caused by increased sympathetic discharge from the central nervous system. Supporting experimen-tal studies have been reported concerning this immediate respiratory consequence, while delayed respiratory consequences with an elevated ICP remain poorly characterized clinically.
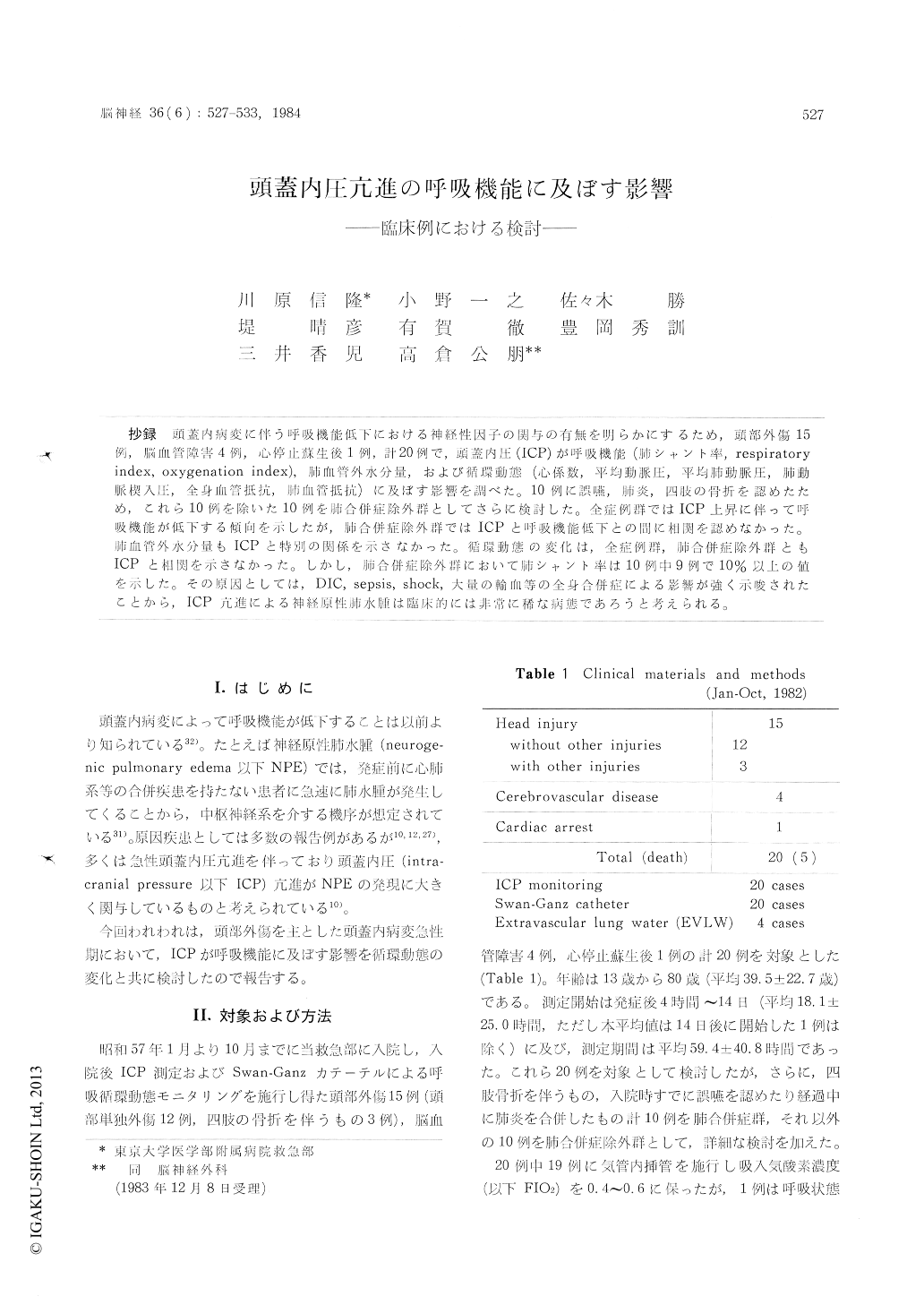
We studied delayed effects of an increased ICP on respiratory functions (pulmonary shunt ratio (Qs/Qt), respiratory index (A-aDO2/PaO2), oxygena-tion index (PaO2/FIO2)), extravascular lung water (EVLW), and hemodynamics [cardiac index (CI), mean arterial pressure (MAP), mean pulmonary arterial pressure (MPAP), pulmonary capillarywedge pressure (PCWP), systemic vascular resis-tance (SVR), pulmonary vascular resistance (PVR)] in 15 cases with head injury, 4 with cerebrovas-cular diseases, and one with hypoxic brain damage. Ten cases had either aspiration, long bone frac-tures (the syndrome of fat embolism), or pneumo-nia, and the 10 cases without these pulmonary insults were defined as the cases without pulmo-nary complications and studied further.
Pulmonary functions deteriorated as the ICP rose in the total cases, but in the cases without pulmo-nary complications, the correlations between the pulmonary functions and the ICP were not signi-ficant. None of the hemodynamic parameters cor-related with the ICP in both the total cases and the cases without pulmonary complications. In one case the positive correlation between EVLW and ICP was suggested. However, in the other 3 cases EVLW did not correlate with the ICP. Although the pulmonary shunt ratios in the cases without pulmonary complications did not correlate with the ICP, they were generally higher than normal. As the causes of these, various systemic complications such as DIC, shock, blood transfu-sion, sputum production etc. were suggested to have impaired the pulmonary functions.
As these various kinds of clinical complications may affect respiratory functions with time, respir-atory dysfunctions can not be attributed directly to an increased ICP in clinical settings. In conclu-sion, pulmonary insufficiencies suggesting neuro-genic mechanism were not observed in our series of 20 cases and it could be said that neurogenic pulmonary edema following an increased ICP is a rare disorder when various systemic and pulmo-nary complications were excluded in a strict sence.
Copyright © 1984, Igaku-Shoin Ltd. All rights reserved.


