Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
脳浮腫は種々の脳障害に随伴する重要な病態で,これまでにも脳腫瘍や脳の外傷に伴う浮腫の発生病理と治療が研究されてきた(Galicich,1961, Klatzo,1973, Long,1970,Pappius,1963,Pappius,1969)6,11,15,18,19)。脳の虚血に続発する脳梗塞にも,死因となるほどの浮腫が随伴する場合があるが,その発生および消退過程はきわめて複雑で,グルココルチコイドの効果についても相反する報告がなかばしている(Harrison,1972,Plum,1963)8,20)。一方,いかなる脳障害に起因するのであれ,いつたん浮腫および腫脹が発生すると,二次的に周辺の脳は圧排されて虚血状態に陥るので,この意味においては,虚血脳と脳浮腫の関係は,浮腫の原因にかかわりなく,ある程度共通して存在する。
脳を灌流する大血管の血流を遮断して脳の一部に虚血状態を作ると,高分子に対する脳血管壁の非透過性は,すぐには障害されない(Olsson,1971)17)が,脳浮腫は早い時期から認められる(Yamaguchi,1976)24)。この早期浮腫の性格は十分に分つておらず,また,血液—脳関門が破綻する時期の前と後に出現する浮腫の相対的重要度も知られていない。最近,虚血にもとづく神経細胞の死滅過程・血液—脳関門・脳浮腫の三者の密接な相互関係が少しずつ解明されつつある中で,我々は,脳のfocalischemic infarctionの過程で発現する浮腫を化学的立場から分析する日的で,以下の実験を行なつた。
Cerebral edema was studied from chemical aspects in the course of development and advancement of ischemic cerebral infarction. Sequential changes of water, sodium, and potassium contents, in addition to fresh weight of cerebral hemispheres, were measured in gerbils following unilateral transection of common carotid arteries. The behavior ofcerebral blood vessel permeablity to serum albumin was also evaluated by the use of Evans blue tracer.
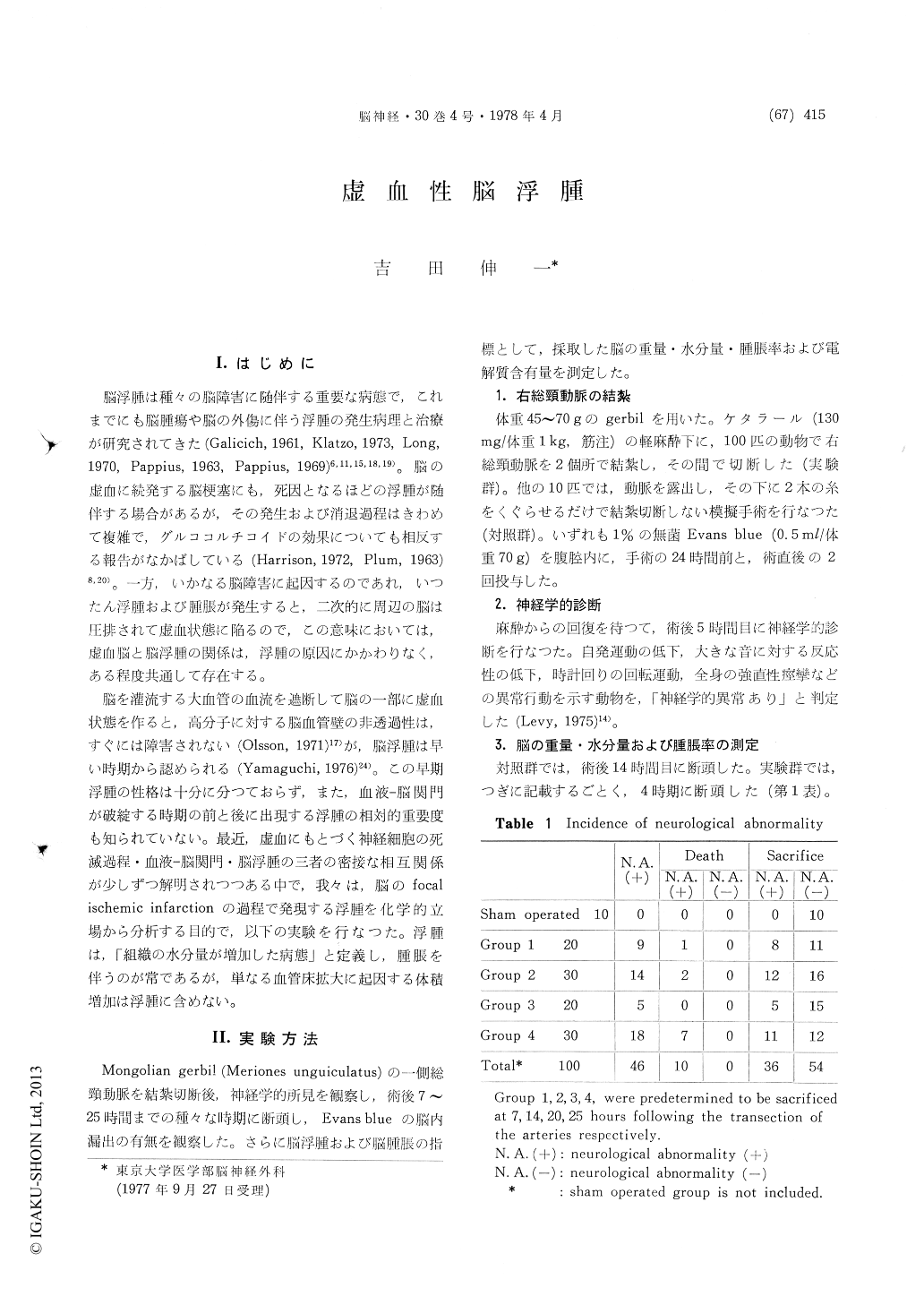
Neurological abnormality was detected in 46 percent of animals. In neurologically normal animals, the cerebral vessels remained impermeable to Evans blue and the edema did not develop. In neurologically affected animals, the edema was present as early as 7 hours from the onset of ischemic stress, and continued to progress in spite of the absence of Evans blue extravasation. By the time of 25 hours after the onset of ischemic stress, however, the ipsilateral cerebral hemisperes became stained blue with the dye in half of the neurologically affected animals. Chemical changes manifested in the neurologically affected animals were: an increase in the water content accompanied with a volume increase, an increase in the sodium content, and a decrease in the potassium content. The severest change per unit time has taken place in the initial 7 hours in each parameter. This indicates rapidly progressive failure of water and electrolyte regulation in the brain at the early stage of cerebral ischemia. The early cerebral edema observed in the ipsilateral paramedian portion of the brain where usually escapes from anatomical infarction suggests that similar pathophysiological process occurs in the adjacent area of the ischemic center, and these water and electrolyte disturbances are potentially reversible. A relatively small amount of the edema and swelling was additionally intro-duced following the development of the abnormal cerebral vessel permeability to serum albumin.
The ischemic brain edema has two distinct com-ponents. The first component is the one which starts to develop early and is independent of the permeability change in cerebral blood vessels tomacromolecules. It probably reflects metabolic dysfunction of glia and neurons in the face of energy deficiency, and the site of fluid accumulation may be intracellular in nature. The second com-ponent appears late, and results from incompetence of the cerebral vessels which are no longer im-permeable to macromolecules. Direct injury to endothelial cells is probably responsible for the passage of macromolecular substances through the vessel walls. Extravasation of plasma can cause extracellular fluid accumulation in the brain parenchyma. However, considering that the median survival time of the neurologically affected animals is about 30 hours, the first component of the edema is assumed to be quantatively of primary importance in this model.
This study presents intimate but complex inter-relationship between tissue necrosis and edema in the dynamic processes of ischemic cerebral infarction. In response to ischemic stress, potentially reversible cerebral edema presumably based on cellular swelling of the affected brain parenchyma occurs first. The edema and swelling progresses further with the development of tissue necrosis in the absence of the alteration of the blood-brain barrier characteristics to macromolecules. When the cerebral vessels become incompetent at the advanced stage of ischemic cerebral infarction, the additional edema is introduced into the necrotic brain parenchyma by the leakage of various plasma components. At this stage, on the other hand, tissue loss of the necrotic brain becomes recogniz-able. The final feature of the ischemic cerebral infarction is localized cerebral atrophy, since cerebral edema is of a trasitory nature.
Copyright © 1978, Igaku-Shoin Ltd. All rights reserved.


