Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
脳組織は他臓器にくらべて酸素消費量が大きいため,脳循環障害により脳hypoxiaにおちいると,すみやかに不可逆性変化を生じ,その結果,重篤な神経脱落症状を呈してくる。従つて,脳虚血発作急性期における虚血脳局所循環と代謝の変化を適確に把握することは,重要な課題である。
最近の脳循環代謝検査法の進歩は,脳虚血急性期における虚血脳局所を中心とした脳循環と代謝の変化を次第に明らかにしてきたが,一方,さらに複雑な問題を提起したのも事実である。すなわち,脳虚血急性期における虚血脳局所血流と代謝の解離4)あるいは,虚血脳周辺部に認められる脳腫脹,脳浮腫による組織圧の上昇と脳循環の関係など,新たな問題が提起されている2)。
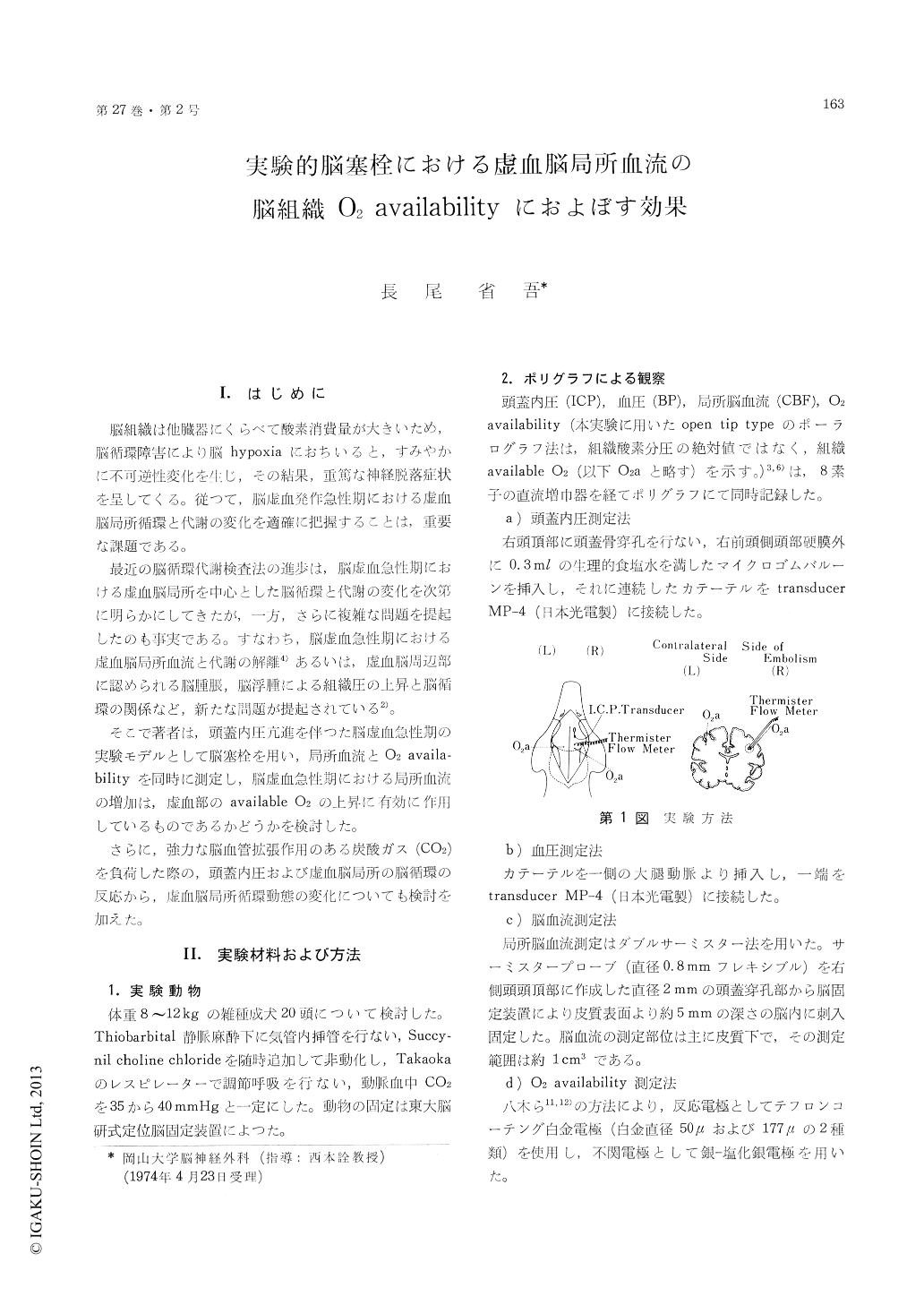
O2 availability (O2a) of cerebral tissue and regional cerebral blood flow (rCBF) as well as intracranial pressure and blood pressure were studied in 20 dogs following injection of varying amounts of room air and Macroaggregated albumin (M. A. A.) into the right internal carotid artery.
O2a was measured by the polarographic method at the depth of 5 mm below the cerebral surface which was within the range of measurement of rCBF.
Following air and M. A. A. embolism, there was an increase of rCBF in all animals but the responses of O2a were classified into three types depending on the duration of ischemia at the site of O2a measurement. In type Ⅰ, O2a was decreased for 5 to 6 minutes following the embolism but restored to a level before the embolism (5 dogs). The vas-cular occlusion due to embolism in this type was considered to be extremely transient.
In Type Ⅱ, the duration of decreased O2a after embolism was longer, i. e., 15 to 20 minutes (4 dogs). It was noticed during the observation of cortical vessels that the duration of O2a decrease in this type corresponded to that of resolution of the embo-lic state with air and M. A. A.
In these two types, O2a was increased in propotion to the increment of cerebral blood flow by CO2 in-halation after the embolism.
It was presumed that a transient ischemia occur-red by air and M. A. A. embolism in those groups and that the administration of a vasodilator such as CO2 caused an increase in 02a as well as in cerebral blood flow, being effective for the damaged brain.
In type Ⅲ, in which much more emboli were used than Types I and II, O2a was decreased over the prolonged period of time in spite of the increase of blood flow in the embolic brain (11 dogs). This was probably due to the persistence of ischemic part with low O2a, even after washing out of emboli.
In this group, intracranial pressure increased from 40 to 70 mmHg. Both the changes of intracranial pressure dependent on blood pressure and the di-minished CO2 reactivity of cerebral vessels implied the decrease of vasomotor tone.
In Type Ⅲ, the increment of cerebral blood flow by CO2 inhalation could not increase O2a in the ischemic part, suggesting that this increment of cerebral blood flow would not perfuse the ischemic part effectively.
Furthermore, this increased cerebral blood flow would increase intracranial pressure which results in non-beneficial effects upon the ischemic brain.
Copyright © 1975, Igaku-Shoin Ltd. All rights reserved.


